 I have had some conversations with pharmacists who are on a pay for performance metric program based on this program and they don’t like it. The big reason is the data that is provided to them is flawed. The program finds information around the web about patients and combines it into a report that pharmacists must look up. In addition they need to fix the flawed data that is reported. You are probably not aware of this program as a patient but it exists and it is full of flawed data, being that you are reported as being non compliant if it does not located enough data about you.
I have had some conversations with pharmacists who are on a pay for performance metric program based on this program and they don’t like it. The big reason is the data that is provided to them is flawed. The program finds information around the web about patients and combines it into a report that pharmacists must look up. In addition they need to fix the flawed data that is reported. You are probably not aware of this program as a patient but it exists and it is full of flawed data, being that you are reported as being non compliant if it does not located enough data about you.These scores are being sold to pharma and to insurance companies. Yesterday I read an article that just about made me choke, with an executive being quoted as saying “don’t waste your time on this patient, spend more time on this one as they show they are taking their medications”…again here we go again with flawed data. You can look at the link below to see an actual conversation I had with a pharmacist and how this works. They hate it as the executives from the EQuiPP program are constantly breathing down their backs as the pay for performance numbers are not improving fast enough, when in fact the data is not correct. Patients who pay cash are being classified in error as Outliers.
Patients Who Pay “Cash” When Filling Prescriptions Are Now Called “Outliers, Pharmacists Required to Fix Outliers as They Show Up As Non Medication Adherence Compliant With 5 Star Systems Full of Flawed Data…
Do you not think these flawed scores will be used to deny or allow access? Better think on that one again. We know CMS is having a hard time today with many of their models with flawed data and in turn not improving care to the patient. Also, don’t confuse medication prediction scores with “actual” facts that PBMs use to see who’s filling their prescriptions. Those are actual transactions that have taken place where most of the predictions scoring is pure bullshit.
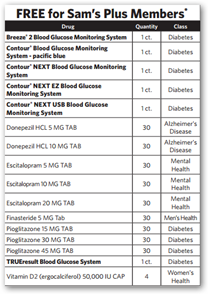
We know CMS is having a hard time today with many of their models with flawed data and in turn not improving care to the patient. Also, don’t confuse medication prediction scores with “actual” facts that PBMs use to see who’s filling their prescriptions. Those are actual transactions that have taken place where most of the predictions scoring is pure bullshit. CMS Medicare Part D Program With Medication Therapy Management–Here Comes the Flawed Medication Adherence Prediction Scores, Make Sure Jane Doe Gets the “Cheap Meds”..
All pharmacy benefit managers today are using some kind of prediction scoring and just take a look at the screenshot right off the Express Scripts page to the right here. Do you see open discrimination here? You should as they use 300 “secret” metrics created by some algorithm to give you a “secret” score that you can’t have or see. If the code were ever broken down so we could see the metrics here I’m sure you would see all kinds of queries related to race, etc. as you can already see one in the image for “income” and “age” if under 65 years old. You are being scored on many things you can’t change which is not fair.Medication Adherence Predictions Enter the World of Quantitated Justifications For Things That Are Just Not True, Members of the Proprietary “Code Hosing” Clubs Out There Destroying Your Privacy
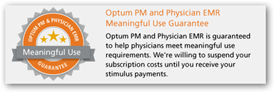
All of this “scoring” costs lot of money and in healthcare today, we are paying for tons of predictive queries and software platforms that offer little or no ROI and this is a big one. We come right back to Excess Scoring of US Consumers and we get no benefit at all. Here’s some additional links below if you want to catch up on what’s going on today with all of this. Pretty much all of this goes back again to a division of Untied Healthcare, called Ingenix, which is now Optum Insights which created such “scoring” of patients as that’s what they do. In addition, you can find some shocking “Cronyism” political ties here that might help make more sense of what’s going on and who’s pocket all of this is feeding.FICO Medication Adherence Scoring Should Be Banned As It’s Quantitated Justifications for Profit That Hurts US Consumers Using Proprietary Algorithms That Cannot Be Replicated For Accuracy or Audited
Express Scripts- New Program to Contact and Predict Patients Who May Not Be Taking Their Medicine Based On Ingenix Algorithms–We Want the Revenue Please Don’t Stop
All in all, predictive medication scoring also helps pharma substantiate the high prices of their drugs as for years it’s been a media circus of “keep blaming the patient” for non perfect results. I learned that tidbit from a former executive and code writer at the NISS many years ago. Anyway, pay attention here is this is what your pharmacist does today for their performance metrics, dealing with the flawed data that comes down the line. Former President Jimmy Carter made a speech not too long ago about the US not being a democracy any more and how now is becoming more of a dictatorship and here’s one big example of how this works with using algorithms and flawed data created by coders and developers to control individuals in the US. BDCAMP HILL, Pa.--(EON: Enhanced Online News)--Rite Aid Corporation (NYSE: RAD) announced today that pharmacists across its nearly 4,600 locations chainwide are now utilizing Pharmacy Quality Solutions’ (PQS) EQuIPP, an information management platform that provides access to performance data across key patient care quality metrics, including those focused on medication adherence and appropriate medication use. Rite Aid is the largest drugstore chain to provide EQuIPP access to all pharmacists.
“Value-based healthcare is here to stay and that’s why it’s important for Rite Aid to provide our pharmacists with the resources and tools they need to deliver improved health outcomes for their patients,” said Jocelyn Konrad, Rite Aid executive vice president of pharmacy. “Our pharmacists are committed to providing excellent care to their customers, and with EQuIPP, we’re empowering them to make an even greater difference in the health and wellbeing of their customers and succeed in today’s healthcare environment.”
http://www.enhancedonlinenews.com/portal/site/eon/permalink/?ndmViewId=news_view&newsId=20151216005752&newsLang=en&permalinkExtra=Rite-Aid-Pharmacists-EQuIPP-Platform-Measure-Patient-Focused
 to administer treatments at home versus making a trip to the hospital or to the doctor’s office. This is yet one more subsidiary added to the approaching 400 or so subsidiaries of United Healthcare, and of course this is one is “tiered” under the Optum subsidiary.
to administer treatments at home versus making a trip to the hospital or to the doctor’s office. This is yet one more subsidiary added to the approaching 400 or so subsidiaries of United Healthcare, and of course this is one is “tiered” under the Optum subsidiary.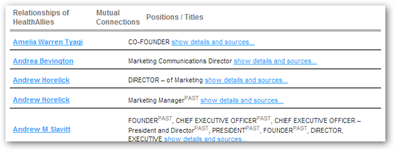
 given the job of being head Global Health Initiative from Obama and that project failed after a couple of years and was dumped. Here’s a background summary of how Ingenix operated under the leadership of Andy Slavitt and all the lawsuits filed over the use of their algorithms.
given the job of being head Global Health Initiative from Obama and that project failed after a couple of years and was dumped. Here’s a background summary of how Ingenix operated under the leadership of Andy Slavitt and all the lawsuits filed over the use of their algorithms. 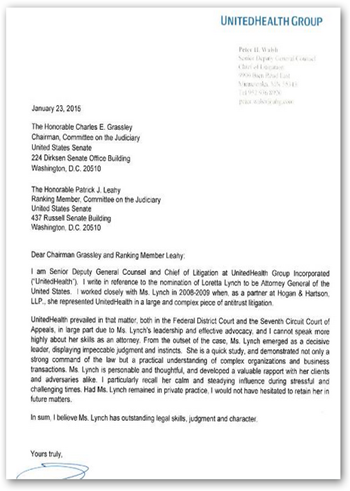 who also has been elected to the
who also has been elected to the  their data. So far all we have had of any significance reported is the same thing Kaiser reported from their registry information on hip and knee replacements. A big part of how Optum makes their money is selling data and access to data. What’s really interesting is that the same type of data mining operation was set up at the FDA and it in turn gets very little press, the agency that approves the drugs and devices that are allowed to be sold in the US.
their data. So far all we have had of any significance reported is the same thing Kaiser reported from their registry information on hip and knee replacements. A big part of how Optum makes their money is selling data and access to data. What’s really interesting is that the same type of data mining operation was set up at the FDA and it in turn gets very little press, the agency that approves the drugs and devices that are allowed to be sold in the US. letting the Labs use patient electronic medical records. It’s kind of strange that HHS is not even supportive of their own FDA efforts with the Sentinel Data Base, right? Again this goes to show the long time relationship and a bit of cronyism with HHS and United Healthcare as well. If you poke around a bit more than you might read about our current head of the DOJ, Loretta Lynch, she used to represent United Healthcare with anti-trust suits, so you can just about figure she’s do nothing with insurance carriers when it comes to anti-trust, or at least this company. Of course we all may or may not know by now that Secretary Burwell was a former Chief of Staff for Bob Rubin that was one of the big three that turned the US economy on it’s ear with abandoning Glass Steagall and furthering the allowance of derivatives in the stock markets. If you want more background on all of that, visit the
letting the Labs use patient electronic medical records. It’s kind of strange that HHS is not even supportive of their own FDA efforts with the Sentinel Data Base, right? Again this goes to show the long time relationship and a bit of cronyism with HHS and United Healthcare as well. If you poke around a bit more than you might read about our current head of the DOJ, Loretta Lynch, she used to represent United Healthcare with anti-trust suits, so you can just about figure she’s do nothing with insurance carriers when it comes to anti-trust, or at least this company. Of course we all may or may not know by now that Secretary Burwell was a former Chief of Staff for Bob Rubin that was one of the big three that turned the US economy on it’s ear with abandoning Glass Steagall and furthering the allowance of derivatives in the stock markets. If you want more background on all of that, visit the 
 nd this is not good with one company having such a huge monopoly. The link below will tell you more about Mr. Slavitt, who President Obama has nominated to run CMS. If you have paid attention to the news in the last few days, he seems very much distracted with social networking comments and just not in touch at all. Seriously why does the President of the US need a personal Facebook page? I see an addiction here perhaps and virtual and real world values being confused.
nd this is not good with one company having such a huge monopoly. The link below will tell you more about Mr. Slavitt, who President Obama has nominated to run CMS. If you have paid attention to the news in the last few days, he seems very much distracted with social networking comments and just not in touch at all. Seriously why does the President of the US need a personal Facebook page? I see an addiction here perhaps and virtual and real world values being confused. 

 she needed as well and those too were sent in bulk. Here’s the
she needed as well and those too were sent in bulk. Here’s the 
 of course. There are other Health Savings Accounts around of course to choose from. Well here we have MasterCard who we should all know by now are just marketing and mining your data to who ever seems to have the money to buy anymore. Here’s a company names Argus, who buys credit card information and then continues on to “score” you. We’re not talking credit scores here, but anything they can think of where they can take data, score you with some query some Rogue software engineer came up with to make money.
of course. There are other Health Savings Accounts around of course to choose from. Well here we have MasterCard who we should all know by now are just marketing and mining your data to who ever seems to have the money to buy anymore. Here’s a company names Argus, who buys credit card information and then continues on to “score” you. We’re not talking credit scores here, but anything they can think of where they can take data, score you with some query some Rogue software engineer came up with to make money. Health Savings Account, which is why they exist is that they are tax free. Most folks get into a Health Savings Account through their employer, although some are available outside those parameters. If you have one at work from your employer, then if you leave, you need to transfer or close the account for the most part.
Health Savings Account, which is why they exist is that they are tax free. Most folks get into a Health Savings Account through their employer, although some are available outside those parameters. If you have one at work from your employer, then if you leave, you need to transfer or close the account for the most part. 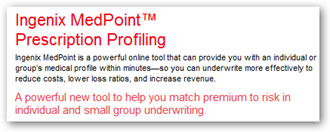 prescription data. As a matter of fact, they licensed and probably still collect a lot of money from this, their algorithms to companies like Express Scripts to “score” you on the flawed Medication Adherence Prediction Metrics which are totally discriminatory as the metrics are secret and you can’t see them. The name Ingenix, at least in the US has now been changed to Optum.
prescription data. As a matter of fact, they licensed and probably still collect a lot of money from this, their algorithms to companies like Express Scripts to “score” you on the flawed Medication Adherence Prediction Metrics which are totally discriminatory as the metrics are secret and you can’t see them. The name Ingenix, at least in the US has now been changed to Optum.  was recently settled. Andy Slavitt, who is currently running CMS was the brainchild here and is a former Goldman Sachs banker who was the CEO and ran the Ingenix subsidiary of United Healthcare for years. Why Obama nominated him for the job full time is beyond me, but as of now he’s “acting” as the chief administrator. See how this all ties together with old Mr. Slavitt leading the way to connecting health insurance to banking? The Optum bank has been around for a while and is located in Salt Lake City.
was recently settled. Andy Slavitt, who is currently running CMS was the brainchild here and is a former Goldman Sachs banker who was the CEO and ran the Ingenix subsidiary of United Healthcare for years. Why Obama nominated him for the job full time is beyond me, but as of now he’s “acting” as the chief administrator. See how this all ties together with old Mr. Slavitt leading the way to connecting health insurance to banking? The Optum bank has been around for a while and is located in Salt Lake City.  United bought the company, it became a subsidiary of United Healthcare, so there you go. The company is now a subsidiary of the huge too big to fail health insurer, who actually gets 2/3rds of their revenue from insurance policies and the rest from selling software and algorithms for a big chunk of the other third.
United bought the company, it became a subsidiary of United Healthcare, so there you go. The company is now a subsidiary of the huge too big to fail health insurer, who actually gets 2/3rds of their revenue from insurance policies and the rest from selling software and algorithms for a big chunk of the other third. United wrote to Grassley to make sure she got approved. You almost have to laugh at when she says she’s going after Wall Street bankers who are indeed much smarter than her and can code her right under the table with her using legal verbiage only, been going on in this country for years. The code hosers are in control.
United wrote to Grassley to make sure she got approved. You almost have to laugh at when she says she’s going after Wall Street bankers who are indeed much smarter than her and can code her right under the table with her using legal verbiage only, been going on in this country for years. The code hosers are in control.
 and thus so, if consumers want their medical bills paid with a larger dollar amount, they go there. The research needed here is to find the doctors and hospitals who are in network. As a matter of fact insurers make it harder for you all the time to research as their own systems are so complex, they have a hard time breaking it down for the consumer to research with firing doctors all the time with quant manufactured models that pretty function like financial models.
and thus so, if consumers want their medical bills paid with a larger dollar amount, they go there. The research needed here is to find the doctors and hospitals who are in network. As a matter of fact insurers make it harder for you all the time to research as their own systems are so complex, they have a hard time breaking it down for the consumer to research with firing doctors all the time with quant manufactured models that pretty function like financial models. 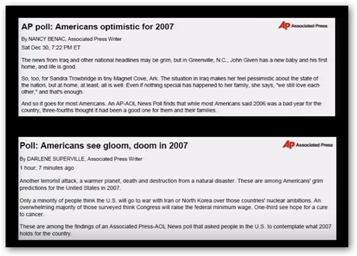 sense as if I don’t get enough, my body tells me, so what’s so difficult about that? Sure there are real problems with people who for what ever reason “can’t sleep, but that’s a different issue all together. Are you going to spend all this time and clutter your mind with how much sleep you need to in turn become much more insecure as all the media tells you to do this? It’s pretty much what’s going on to where you can’t make a simple determination of whether or not you are getting enough sleep, which has pretty much been common sense.
sense as if I don’t get enough, my body tells me, so what’s so difficult about that? Sure there are real problems with people who for what ever reason “can’t sleep, but that’s a different issue all together. Are you going to spend all this time and clutter your mind with how much sleep you need to in turn become much more insecure as all the media tells you to do this? It’s pretty much what’s going on to where you can’t make a simple determination of whether or not you are getting enough sleep, which has pretty much been common sense.  but it’s a useless piece of garbage report as it entails nothing about what hospitals were “available” in network or the cost..so again, dump their studies and you can read the link below as what they do is just junk outside of giving you an address and phone number for a doctor or a hospital. I found my former MD who had been dead for 8 years listed on their site an still seeing new patients. The use of their site for credible research is like out the window and don’t waste your time. Word of mouth with doctors and hospital selections still seem to be at the top and for good reason.
but it’s a useless piece of garbage report as it entails nothing about what hospitals were “available” in network or the cost..so again, dump their studies and you can read the link below as what they do is just junk outside of giving you an address and phone number for a doctor or a hospital. I found my former MD who had been dead for 8 years listed on their site an still seeing new patients. The use of their site for credible research is like out the window and don’t waste your time. Word of mouth with doctors and hospital selections still seem to be at the top and for good reason.