To help fight fraud, your healthcare claim could be getting a big “score”. In other words we are once again depending on those algorithms to determine what could be determined as fraud. If your claim gets a “big” score, then perhaps the red tape and battle is on. This is somewhat the same technology that is used by the banking industry; however, in healthcare items are not as cut and dry, thus we will have even more calculated and derived algorithms to better mine the functionality of this process.
be determined as fraud. If your claim gets a “big” score, then perhaps the red tape and battle is on. This is somewhat the same technology that is used by the banking industry; however, in healthcare items are not as cut and dry, thus we will have even more calculated and derived algorithms to better mine the functionality of this process.
Insurers state they do not use these algorithms to deny claims, but rather bring it to the attention of someone to review, and well we all know what that means, delay and whatever else comes down the tubes there to prove that the claim is legitimate, regardless of what type of “score” the algorithms produced. This is known as a “false positive” where you may have to somewhat prove your authenticity and innocence and the fact that you need care!
Once a fraud investigation begins, forget HIPAA, as there is no privacy here and the investigating process does not protect your medical records as they become part of the investigation process, and contractors are required to meet HIPAA compliance, so when your medical records are viewed with an fraud investigation, who gets to see them? The information is supposed to ignore names, social security numbers, etc. but one fraud program from Ingenix included the patient address to score to see if the patient is traveling to receive medical care, one additional parameter used to create the “score”.
Are We Ever Going to Get Some Algorithm Centric Laws Passed for Healthcare!
As a physician, if you want to see how much information is out there on the web about yourself, sign up for the free NEPSI e-prescribing program and you will be presented with a number of questions to answer to ensure that it is in fact really you signing up. You will see questions that ask about where you lived 20 years ago and perhaps even names of individuals you know present and in the past that pretty much only you will know
the answers to, this is data mining and is actually a good thing to prevent someone fraudulent from signing up, but on the other hand, welcome to internet data mining, an eye opener. I have had this conversation with a few physicians that were amazed at what was presented in the way of questions.
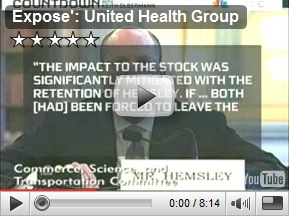
In a related video, Keith Olbermann takes a look at healthcare reform and traces back the history of Mr. Hensley of United Healthcare and the Arthur Anderson connection where he was formerly employed along with the back dated stock options where investors sued twice on this issue. Also discussed is the losing proposal of “co-ops”. We learned that lesson a long time ago in California. I watched “co-ops” become useless in another industry, logistics, a number of years ago as marketing and sales strategies changed, the participating companies just would come in and cut the rates of the “co-op” to a lesser amount, so there went the pricing benefit. Also, the way the “co=ops” were formulated in logistics and worth a mention is that they were a “non profit” organization and all members were also responsible for any legal actions and debt too. I am not totally familiar with the way they are being proposed in healthcare, but if this item is included, beware of one more snag with a “co-op” proposed solution. BD
Goldman Stolen Code – Has Algorithmic Fraud Become A Business Model in HealthCare Too?
The political pressure to reduce health care costs is forcing many health insurance companies to reconsider how they detect and combat fraud. Health insurance fraud is estimated to cost insurers at least $68 billion to $70 billion a year, or 3% of total health care spending,
according to the National Health Care Anti-Fraud Association, or NHCAA, an industry group. (Fraud includes health care providers billing insurance companies for procedures that were never performed, performing services that are not medically necessary or overcharging for services.)
To detect fraud, insurers have historically used a so-called pay-and-chase method: They reviewed claims after paying them, and if fraud was suspected, they tried to recover their money. It was no easy task -- the worst case scenario could involve expensive collections efforts or lengthy courtroom battles.
Claim Denied? Health Fraud Score May Be to Blame at SmartMoney.com
Related Reading:




serv-U-well pharmacy adress is 18250 W warren st Detriot Mi.481 that Dr Abid and his assistnet Husain have been sharening prise of the medicine with patient
ReplyDelete