It’s all about money and this pretty much says it all.  When you look and compare health insurance companies there’s not one as big as United with the “huge” daily chain of subsidiaries that keeps growing at a pretty rapid speed. Most consumers don’t see the entire package here on how health insurance companies operate and make their money, they only look and think about insurance policies, which of course is the first item to look at, but when you dig beyond the first area of business you will find a lot more.
When you look and compare health insurance companies there’s not one as big as United with the “huge” daily chain of subsidiaries that keeps growing at a pretty rapid speed. Most consumers don’t see the entire package here on how health insurance companies operate and make their money, they only look and think about insurance policies, which of course is the first item to look at, but when you dig beyond the first area of business you will find a lot more.
The CEO states they will participate only in exchanges that are “fair” and the company far outreaches every other insurer out there  with the use of analytics and has for years. You can go back to the AMA lawsuit to where United short paid hospitals and doctors for 15 years and I believe the checks are either or on the way back to doctors or it is soon to happen. They made money both ways here as they also licensed the analytics data base to other major insurers so you had Blue Cross, Health Net, Cigna and more jump on the same bandwagon and they short paid as well using the United numbers. This fact in itself makes it very difficult to fully trust some of the reports and studies they create as the CEO had said many times “the shareholders will prosper” and how many of them I wonder are insured by United? It’s just a question that rambles around in my head and for this reason alone you do have to keep your eyes open as everything analytically may be as it seems.
with the use of analytics and has for years. You can go back to the AMA lawsuit to where United short paid hospitals and doctors for 15 years and I believe the checks are either or on the way back to doctors or it is soon to happen. They made money both ways here as they also licensed the analytics data base to other major insurers so you had Blue Cross, Health Net, Cigna and more jump on the same bandwagon and they short paid as well using the United numbers. This fact in itself makes it very difficult to fully trust some of the reports and studies they create as the CEO had said many times “the shareholders will prosper” and how many of them I wonder are insured by United? It’s just a question that rambles around in my head and for this reason alone you do have to keep your eyes open as everything analytically may be as it seems.
Outpatient Surgery Centers File Class Action Lawsuit Against UnitedHealth and Ingenix for Underpayments
Ingenix Data Base Has Some Long Reaching Legal Tentacles with Aetna, Blue Cross, Blue Shield, Humana
If you don’t understand how health insurance works these days, read up on the web and listen to the quarterly reports and that will give you an idea of all the various entities owned and acquired by the insurers, and again United far ahead of any of the rest of them with a huge focus on analytics and all kinds of other companies. You can use the words “subsidiary watch” on this blog and find an army of them with all carriers. You now find United with “retail” stores popping up in the US too. One executive from the company made a comment recently about what buying insurance can’t be more like a bank with tellers, and United has a bank come to think of it with over a billion on deposit from health savings accounts that allows them to make loans and conduct other types of financial investments with the money. I posted this back in 2010 and the money on deposit could have grown since then.
days, read up on the web and listen to the quarterly reports and that will give you an idea of all the various entities owned and acquired by the insurers, and again United far ahead of any of the rest of them with a huge focus on analytics and all kinds of other companies. You can use the words “subsidiary watch” on this blog and find an army of them with all carriers. You now find United with “retail” stores popping up in the US too. One executive from the company made a comment recently about what buying insurance can’t be more like a bank with tellers, and United has a bank come to think of it with over a billion on deposit from health savings accounts that allows them to make loans and conduct other types of financial investments with the money. I posted this back in 2010 and the money on deposit could have grown since then.
UnitedHealth Group Owns a Bank With Deposits Surpassing a Billion – OptumHealth Bank FDIC Insured
I don’t know how analysts can theoretically compare United to other insurers if you look at the entire corporation as a whole as they are far more complex and own more entities than the rest. When you read the latest reports about their profits slipping 1%, let’s not forget the outlay of money spent to buy the biggest managed care companies in Brazil for one example. The company is making more money “managing” care these days and again this comes back to extreme use of analytics and algorithms modeled for profit.
United Healthcare Negotiated to Buy 90 Percent of the Largest Managed Care Provider in Brazil, Where Insurers Can Own Hospitals and Physician’s Practices
They also get patents for a lot of their developed technologies and this leaves the door open to of course sell such to many to include other insurers for one. Next time you take one of their surveys, remember it’s patented and probably available for other companies to license.
QualityMetric/Ingenix (United HealthCare) Receives Patent for Patient Health Survey Algorithms-Subsidiary Watch
United is busy in the medical records business too…..
They are also in the electronic medical records business with selling CareTracker, which is their own EHR developed years ago as well as owning a couple other subsidiaries that produce electronic medical records for sale to doctors, so the company is very much in the EHR business as well. CareTracker can connect to their “clearinghouse” company which used to be a division of Ingenix which now falls under the Optum name. Ingenix and their consulting services have been around for a long time and a big part of their business is selling data for profit. In addition to CareTracker there’s also Optum Insight, a non-web based EHR system. Here’s a few examples below on their electronic medical records and HIE businesses.
records for sale to doctors, so the company is very much in the EHR business as well. CareTracker can connect to their “clearinghouse” company which used to be a division of Ingenix which now falls under the Optum name. Ingenix and their consulting services have been around for a long time and a big part of their business is selling data for profit. In addition to CareTracker there’s also Optum Insight, a non-web based EHR system. Here’s a few examples below on their electronic medical records and HIE businesses.
Ingenix (Subsidiary of United Health Group) Marketing Care Tracker EHR To Community Health Centers–Subsidiary Watch
Axolotl (A Subsidiary of Ingenix) Creates Reporting and Analytics Solution for Health Information Exchanges–Algorithms for HIE–Business Intelligence -Subsidiary Watch
ClickFreeMD Selling Software EHR, Practice Management Bundled Records Solution–Emphasis on AMA Endorsement And Software “Powered” by Ingenix–Tethered or Untethered
Occasionally they do sell some assets such as this one below which was in the clinical trial business and created their Life Sciences division.
Ingenix (Subsidiary of United Health Group) Sells i3 Clinical Trials And Creates Life Sciences Group-Subsidiary Watch
There’s also the company China Gate they bought a couple of years ago that works to promote Chinese drugs and devices in the US and worldwide.
UnitedHealth subsidiary (Ingenix Subsidiary I3) Acquires ChinaGate – Working to Sell Chinese Products Globally
Also on that note they have yet another consulting company that also consults with drug and device companies here in the US to get them introduced to the FDA and consult on the entire process and you see them regularly at conventions.
company that also consults with drug and device companies here in the US to get them introduced to the FDA and consult on the entire process and you see them regularly at conventions.
United Healthcare (Optum) Owns A Consulting Firm for FDA Drug and Device Approvals, Clinical Trials–CanReg - Subsidiary Watch
For a while it seemed liked almost everything the AMA was offering with electronic records and other software services all began with Ingenix (now Optum) as their initial partner. I’ve been doing this blog for over 4 years now and posted a lot of those entries. Then in February of 2012 the AMA sold their Amagine Project to AT&T. This group continues to market and sell Optum PM and Physician EMR as well as a couple other medical record services. You just wonder how the data and software trails go, or at least I do on who actually wrote and creates some of the software we see out there so when making a purchase I know who’s making money. You might be getting marketed and sold a United Healthcare product and not even know it.
AMA Selling Online Physician Portal to AT&T–The Amagine Project, There’s Money in Selling And Aggregating Those Algorithms
Also in the area of medical records United with their Optumsight division is working with Epic Medical records and they went out and created a whole new company that is a clearinghouse (algorithms and analytics) to integrate there being that Epic is installed in so many large hospital systems, not to want to miss a part of the pie here.
OptumInsight (A Wholly Owned Subsidiary of United HealthCare Optum Division) Creates Medical Clearinghouse Integrated With Epic Practice Management Software-Subsidiary Watch
The company does seem to have an inside advantage that  other insurers do not have with the hiring of Steve Larson from HHS who was accredited with writing most of the healthcare law and now he sits over at Optum as vice president..so many in key positions as such have left HHS and we are just lucky someone convinced Todd Parks to go to work there when he did as healthcare is so much about analytics and business intelligence today to where even the medical records systems push payer representation first instead of user interfaces for doctors. The company also has various incentives in place all throughout healthcare like this one with Walgreens to where pharmacists can make a little pocket change in some areas of the US. United also has their own internal pharmacy benefit manager too so no battles there like other insurers have with drugs and prescriptions as when you own the place, you direct it.
other insurers do not have with the hiring of Steve Larson from HHS who was accredited with writing most of the healthcare law and now he sits over at Optum as vice president..so many in key positions as such have left HHS and we are just lucky someone convinced Todd Parks to go to work there when he did as healthcare is so much about analytics and business intelligence today to where even the medical records systems push payer representation first instead of user interfaces for doctors. The company also has various incentives in place all throughout healthcare like this one with Walgreens to where pharmacists can make a little pocket change in some areas of the US. United also has their own internal pharmacy benefit manager too so no battles there like other insurers have with drugs and prescriptions as when you own the place, you direct it.
UnitedHealthCare To Use Data Mining Algorithms On Claim Data To Look For Those At “Risk” of Developing Diabetes – Walgreens and the YMCA Benefit With Pay for Performance Dollars to Promote and Supply The Tools
Selling data again is also right up there in areas of profit for the company with Ingenix, now Optum with prescription profiling. 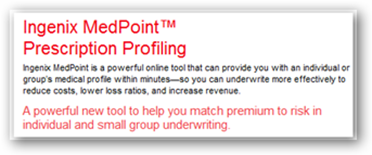 You might guess where some of this comes from if you own the pharmacy benefit manager and work with various drug stores across the US as data selling is a huge profitable business today making billions in profits for all kinds of companies and I keep using the Walgreen example of 2010 where they made short of $800 million selling data only.
You might guess where some of this comes from if you own the pharmacy benefit manager and work with various drug stores across the US as data selling is a huge profitable business today making billions in profits for all kinds of companies and I keep using the Walgreen example of 2010 where they made short of $800 million selling data only.
Also noted on the quarterly report was the revenue anticipated from the new Tri-Care contract which took a few years to settle and United was determined to get one of them through a process of appeals and when that didn’t happen they sued the Department of Defense to get the last unit, the west coast and the current contractor owned by Blue Cross will be going out of business as the loss was not sustainable and United is buying up or contracting with some of the data processing companies that subsidiary owned.
Tri-West Won’t Challenge Tri-Care Military Contract Loss To United Health - Legal Decisions & Contract Awards Allow Machines To Move Money for Profit As Company Will Likely Close Down-Subsidiary Watch
Update: UnitedHealthcare Sues Department of Defense Over Tri-Care Contracts–They Said They Would Do This – Is This A Case Of My Algorithms Are Better Than Yours?
United HealthCare Awards Contract to One Blue Cross/Blue Shield Subsidiary to Process Tri-Care Claims While The Other BlueCross BlueShield Company Lost the Over All Tri-Care Bid To United In the West
Anesthesia management in the hospitals, they are represented here as well with yet another subsidiary.
Ingenix (Subsidiary of UnitedHealthGroup) Buys Picis Hospital Software Analytics Company – Algorithms of Healthcare Continue To Grow
VA Awards Contract to Picis, Subsidiary of Ingenix for Anesthesia Record Keeping Software
The company has also purchased some very large physicians groups in the US and a couple right here in the OC where I live and crying towels were out on this one.
United Healthcare Acquisition of Monarch Healthcare HMO Already Causing Confusion and Access Problems for Blue Shield Patients in Orange County
Now you would have to be living under a rock today not to at least think about the data resources of all of this the the potential they have to run all kinds of analytics and reports and create them for profit, but again remember the company is traded on the open market. A while back I also pondered this question with the loss or gain of business with one entity and with the use of some analytics, does this tend to outpace what other insurers can do with having the ability to run metrics across all kinds of subsidiaries to look for both sales and profit availabilities? In other words if business is lost from one subsidiary is it then absorbed by another and where? I think that’s a good question to ask.
Subsidiary Watch-Corporate Conglomerate Insurers Reduce Compensation Contracts Using One Subsidiary Then Market Same MDs With Another Subsidiary in Health IT
Recently in the news the Mayo Clinic and United are working together on a data project out of yet another new United subsidiary, Optum Labs to run data comparisons with both clinical and claim data.  The two have worked together before with United having contracts with Mayo for patients covered by employer provided insurance being able to use their facilities, which began back in 2010. This venture will be crunching data to compare outcomes with money spent. Researchers will get some benefits here in determining how various treatments work on patients, but Mayo the size they are probably have that going for them already. Mayo doesn’t have any ownership in the Optum Labs division so there’s one big hint there with how the information will be formulated and used.
The two have worked together before with United having contracts with Mayo for patients covered by employer provided insurance being able to use their facilities, which began back in 2010. This venture will be crunching data to compare outcomes with money spent. Researchers will get some benefits here in determining how various treatments work on patients, but Mayo the size they are probably have that going for them already. Mayo doesn’t have any ownership in the Optum Labs division so there’s one big hint there with how the information will be formulated and used.
Everyone is looking for those magic formulas that digital illiterate CEOs boast that trillions will be saved, and they don’t get it:) Sure there are savings but it’s not the illustrious dollars they think as technology moves forward, what you save today will be spent on new technologies and drugs tomorrow. Sure people may get a little smarter in identifiable areas for treatment, that’s a given but there’s not this big post of gold to be saved. I have to laugh at reading this over and over in the media. It’s not the great white hope and will improve efficiencies and help United fine tune their profitability with some of this information too.
So coming back around it looks like United running the government here to a degree with picking and choosing their exchanges. It’s too bad that so many of our government entities like HHS, FTC and a few others can’t get their heads around how this game is played with data as it is  not always applicable for decision making when numbers are only crunched. It was kind of embarrassing when HHS accused doctors of “cheating” with billing and even pulled in the Attorney General on the accusation too, with nothing brought to the table and it was a lack of digital mechanical literacy that prompts such “panic” statements. This was embarrassing and it was more than just me on this blog who said so, the tech folks that see right through it just shake their heads and wonder what the heck is wrong with HHS on this one. Myself I had to sit back and remember this is the same agency that saw value with a Facebook contest and believes magical algorithms will totally solve hospital re-admissions:)
not always applicable for decision making when numbers are only crunched. It was kind of embarrassing when HHS accused doctors of “cheating” with billing and even pulled in the Attorney General on the accusation too, with nothing brought to the table and it was a lack of digital mechanical literacy that prompts such “panic” statements. This was embarrassing and it was more than just me on this blog who said so, the tech folks that see right through it just shake their heads and wonder what the heck is wrong with HHS on this one. Myself I had to sit back and remember this is the same agency that saw value with a Facebook contest and believes magical algorithms will totally solve hospital re-admissions:)
HHS and DOJ Send Letters to Hospital Trade Associations Warning of Gaming Billing System Via Use of Electronic Medical Records–Hospitals Just Learned How to Bill Better & Hired Consultants–Case of Being Algo Duped With Numbers?
Also it was poor show with HHS taking on Dr. Hamburg at FDA on a drug decision and looked like pulling rank from what I read in the news. Government has not quite figured out how algorithmically United has their sites on Medicare as they said “we have a good idea on how to handle this and know what’s going on”….
United HealthCare Issues Another Study, This One Telling Government To Aggressively Manage Medical Care For Seniors-An Area Where A Large Chunk of Their Revenue Comes From Today, Managing Care
With this idea of what’s going on, they seemed surprised that the AAFP found they were paying doctors less than Medicare…so do they know what’s going on..probably more than we would guess because they are looking at doctors’ pay as a way of saving money so do they care that doctors in some areas of the US with their contracts get paid less than Medicare and this somewhat fuels the fire that they want to get a bigger slice in some Medicare business as the company is making more money managing care these days than with policies. Of course you need a policy first to manage that person’s care.
UnitedHealthCare Looks at Doctor’s Pay for Savings, Nothing New There Been Doing It for Years But Keep In Mind We Have the Annual Medicare Cut Fix on the Floor Again with Congress–Timing?
The AAFP Confronts United Healthcare On Reimbursements, Some Are Below Medicare Rates In Parts of the US–Payment Algorithms/Formulas Calculated Deep Within IT Infrastructures Do the Job
What I see out of this venture are some new analytics coming out for sale from United in time with “more data” as  that’s what they live for. It will also stand to fill the pipelines with their studies they put out all the time. Last time I took exception to the tone they use too on some of them with subliminal messages telling consumers in so many words that their ill health is at the root of the US Economy when it is not, Wall Street and banks did it and you can’t put the squeeze on consumers for this. There are positive ways to encourage better lifestyles rather than blame shifting and running some of the propaganda they do.
that’s what they live for. It will also stand to fill the pipelines with their studies they put out all the time. Last time I took exception to the tone they use too on some of them with subliminal messages telling consumers in so many words that their ill health is at the root of the US Economy when it is not, Wall Street and banks did it and you can’t put the squeeze on consumers for this. There are positive ways to encourage better lifestyles rather than blame shifting and running some of the propaganda they do.
The media eats it up as it create a sense of panic and let’s face it anywhere you strike a bone people start with the “drama queen” antics and it creates an illustrious sense of distraction from what’s really going on in the business world and corporate structure love it to see all distracted so they go about what and how they want to do their business that way with nobody asking questions. The CEO said it himself a while back:)
“Stephen Hemsley, the CEO of UnitedHealth, is not intimidated. "Leading companies take advantage of disruptive change in the marketplace," he told reporters recently. "Our shareholders will prosper."
This being said, it would not surprise me to see United offering their expertise on the design of exchanges, perhaps? I guess we shall read the news and see if that happens in the near future as they clearly made the point they are only going to participate where it makes money and if the government can’t design it that way I wouldn’t see them at a loss to offer assistance. They would only stand to get stronger with analytics and closer to getting a share of some Medicare business eventually, it’s the way the models and algorithms work. I do hope our government executives smarten up as right now I feel at such a loss from what I read in the news. Who’s running the healthcare system with the data…and insurer or the government? BD
The leader of the nation's largest health insurer warned Thursday not to assume widespread participation from his company in part of health care overhaul's coverage expansion that unfolds later this year.
UnitedHealth Group Inc. CEO Stephen Hemsley told analysts the insurer's involvement in online exchanges that are expected to help millions buy coverage will depend on whether it's financially viable for the company.
"We will only participate in exchanges that we assess to be fair, commercially sustainable and provide a reasonable return on the capital they will require," he said.
http://finance.yahoo.com/news/insurers-may-prove-choosy-overhaul-213021372.html



0 comments :
Post a Comment