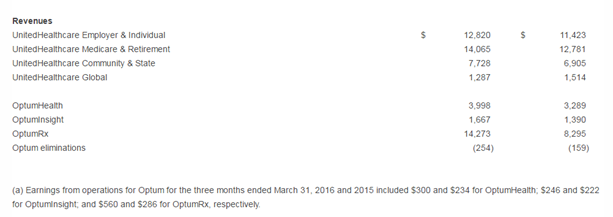
You can read the entire press release here as the report is broken down in several entities, but I found the most striking of all to be the “revenue” section, in other words where the money’s coming from to be of importance. What are we starting to see as the insurer states they are withdrawing from around 8 states with Affordable Care Policies beginning in 2017? The company did not participate in a large way with many of the ACA insurance exchanges and yes a decent number of folks will have to change their plans next year. But what’s the deal with OptumRX revenue? Here’s a screenshot of the revenue numbers and you can look for yourself. The first column is this year and the second column is 2015 for a comparison.
We know that United had a $10 billion dollar bond sale to buy the pharmacy benefit management company, Catamaran that in essence helped get Cigna sanctioned with not being able to sell anymore Medicare Part D policies and I think that restriction is still there today, as the company was denying too many drugs to those insured by Cigna. I had some sources tell me that in some exit interviews, etc. that the Catamaran folks working with referrals and approvals had no idea why they were denying requests other than the fact that the “screen said no” and that ‘s a little scary in itself. In addition, Cigna was supposed to be denied their bonus payments from CMS for a lot of this activity but they gave in and allowed Cigna to get their money from the government. So now all who are insured by Cigna have a pharmacy benefit manager, OptumRX, which is owned by United Healthcare.
CMS Sanctions Cigna-No More Selling Any New Medicare Advantage Policies Until Algo Problems Denying Medical Coverage and Prescription Denials Are Fixed
United Healthcare Having a Big Bond Sale to Finance Purchase of Catamaran Pharmacy Benefit Management Company, Huge 10.5 Billion
United, under the Optum name also bought a Workers Compensation pharmacy benefit management company, who’s largest account just happens to be the US Post Office along with other very large corporations like Southwest Airlines and move…more money.
United Healthcare Buys Helios Workman’s Comp PBM and Their Other Related Businesses
There’s so much money made here on the high prices we pay for drugs that Anthem is suing Express Scripts to get a touch of that money, while at the same time OptumRX is inching its way into Walgreens with a 90 prescription.
Walgreens Signs Agreement With PBM OptumRX (United Heatlhcare) and Anthem Then Sues Express Scripts
The pharmacy benefit management and making money model can be a little complex to understand indeed as the companies get what is called a kickback with sales of the drugs they distribute, and especially on generics, up to 80% can be handed back. It can all add up to a lot of money. So in essence, it may not always be the lowest price drug who gets the contract, it might be the pharma company that offers the biggest percentage kick back. Being United owns OptumRX, this gets a bit tricky as they are there to negotiate drug prices; however, those kickbacks algo go to the United bottom line as profits so the very entity of an insurance company, United, they are there to work for and keep drug prices down, is also the same corporate umbrella that wants all the profit they can get from the pharmacy benefit management company as well. I would think this really becomes a balancing act and this would be where they call in the company quants with math to figure it out for them.
Who knows, a United Healthcare/Optum subsidiary AxelaCare, (bought by the OptumRX subsidiary) may show at your home to administer infusion drug some day as OptumRX bought this company as well. The link below also contains a ton load of cronyism connections that I just felt like adding when I wrote the post. I dug up the CMS director’s relationship to the Elizabeth Warren family and a few money ventures and you can also read how Lorretta Lynch used to handle anti-trust suits for United Healthcare. She’s busy with another job right now and won’t be doing any of that for a while anyway.
OptumRX (United Healthcare) Buys Home Infusion Company AxelaCare-Using Algorithms To Determine Your Care With Being Financed By A “Too Big to Fail” US Health Insurance Company…
For the time being it appears Harken Health, another creation of United Healthcare will stay around for a while with the ACA state insurance policies going away as they put their quants to work to create yet another model of insurance to throw against the wall to see if anything sticks.
United Healthcare Puts Their Quants To Work Again-Designs a Subsidiary to Compete Against Them and Sell Insurance With a New Set of Algorithms Named Harken
The pharmacy software algorithms that help make money selling our data and creating these flawed medication  adherence scores goes way back to 2010 when CMS director Slavitt was President of Ingenix (now renamed Optum) and sold Express Scripts sofware and systems on how to start collecting and selling data on consumers. You do wonder with all of this if we do have the fox minding the hen house today at CMS as it seems ironic that the exact same models, some of which are failing keep working their way from United Healthcare to CMS, i.e. population health which was created by United around 15 years ago with the Ingenix folks. The pharmacy benefit management business has a very profitable side business of selling and scoring all consumers when we pick up our prescriptions and you get secretly scored and sold all the time. If there’s not enough credit card records for them to drag through of yours to see if you filled a presciption, then you default to being an outlier, and if you pay cash, same result.
adherence scores goes way back to 2010 when CMS director Slavitt was President of Ingenix (now renamed Optum) and sold Express Scripts sofware and systems on how to start collecting and selling data on consumers. You do wonder with all of this if we do have the fox minding the hen house today at CMS as it seems ironic that the exact same models, some of which are failing keep working their way from United Healthcare to CMS, i.e. population health which was created by United around 15 years ago with the Ingenix folks. The pharmacy benefit management business has a very profitable side business of selling and scoring all consumers when we pick up our prescriptions and you get secretly scored and sold all the time. If there’s not enough credit card records for them to drag through of yours to see if you filled a presciption, then you default to being an outlier, and if you pay cash, same result.
Patients Who Pay “Cash” When Filling Prescriptions Are Now Called “Outliers, Pharmacists Required to Fix Outliers as They Show Up As Non Medication Adherence Compliant With 5 Star Systems Full of Flawed Data…
Here’s more detail on what’s going on with pharmacy data being sold and how you are secretly scored with proprietary metrics and algorithms that have never been proven for accuracy, but it makes for big money for pharmacy benefit management, sell that data and score those consumers, as pharma and insurance companies are the big buyers. With OptumrX they can give all the scored data away to United as they own them and they’ll probably turn around and “score” you again with the data on some other correlated query.
Medication Adherence Predictions Enter the World of Quantitated Justifications For Things That Are Just Not True, Members of the Proprietary “Code Hosing” Clubs Out There Destroying Your Privacy
The screenshot to the right shows how Express Scripts scores you and again this began in 2010 when Ingenix, now renamed Optum sold them the software needed to begin the scoring processes, when Andy Slavitt, who now runs CMS was the CEO of Ingenix. Below is the back link on that story from 2010, so it revolves back again around one company and their algorithms and analytics, United or one of their subsidiaries.
Express Scripts- New Program to Contact and Predict Patients Who May Not Be Taking Their Medicine Based On Ingenix Algorithms–We Want the Revenue Please Don’t Stop
So the pharmacy benefit managers are all doing it in one shape of an algorithm or another and the data and scored are flawed as now the have started bringing in social network garbage and give you a score that may not accurately represent you at all, but again it’s big money and maybe helps explain the big push by United into pharmacy benefit management. The last quarter revenue tells the story does it not?
you at all, but again it’s big money and maybe helps explain the big push by United into pharmacy benefit management. The last quarter revenue tells the story does it not?
So it’s very interesting is it not to see this huge shift of revenue from OptumRX to even outshadow their insurance group revenues? It beat all of them on it’s own. Of course though if you want information on your doctor or hospital, the last bone thrown at you by United is to link you to the most flawed site on the internet, Healthgrades to find flawed data, survey reviews and other information about them.
By the way, don’t bother with a Healthgrades survey as they tie it to your phone number or email address so they can profile you for more e-commerce behavior analytics and who knows if they are selling that back to United? It seems to be the way it works as we all know Healthgrades is not much more than clickbait for the site to generate ad revenue. You can read below on that topic.
United Healthcare Hits the Bottom of the Barrel Linking Doctor Information to Healthgrades Flawed Data
So what is the future here? Big push into pharmacy benefit management and getting drug kick backs from pharma in the name of lower priced drugs? When do we ever get to see that part of it? Looks like the lost revenue claimed over the ACA insurance policies that are being dropped has been more than replaced, you think? Of course in this process we can all look foward to a lot less privacy, as today’s it is already out of hand. BD



0 comments :
Post a Comment