This is unbelievable if I am reading this correctly as I had assumed that all insurers who licensed the data bases and software from United had agreed to switch to to the new “Fair” data base, but it looks like Horizon Blue Cross/Blue Shield was still using it as that’s part of the settlement here, not to use it anymore. The big AMA court case filed by Cuomo in New York was for 15 years of short paying doctors all across the country. It was not just United/Optum involved here as they licensed it to other insurers, like Aetna who proposed their case at the end of last year for underpaying for around 15 years. Health Net if I remember correctly was one of the first to stop using the data base and settle.
part of the settlement here, not to use it anymore. The big AMA court case filed by Cuomo in New York was for 15 years of short paying doctors all across the country. It was not just United/Optum involved here as they licensed it to other insurers, like Aetna who proposed their case at the end of last year for underpaying for around 15 years. Health Net if I remember correctly was one of the first to stop using the data base and settle.
Now a couple months ago Aetna wants to get out of their proposed settlement o f $120 million and it made notice to the court a week before the hearing. They licensed the same data base and software too. Now a judge is looking at the contract again and if it is found that the doctors have a case, it will go to jury trial. The American Medical Association,the Texas Medical Association, and the medical societies of California, Connecticut, Florida, Georgia, North Carolina, New Jersey, New York, Tennessee, and Washington sued Aetna in 2009 over its use of databases licensed from Ingenix, a UnitedHealth Group Inc. subsidiary. Physicians who have been in business since 2003 and provided out of network services might be able to join this lawsuit. Here’s the back link on the initial settlement announcement of what they are trying to get out of now. Aetna also keeps a number of reinsurance options located in the Cayman Islands as well.
Now back to Horizon Blue Cross Blue Shield, there was no money given here with the exception of payment of legal fees for the class members. It’s also noted that there’s probably an appeal on the menu here too. A Cigna case settled with no money awarded as they too like Health Net stopped using the data base and agreed in 2009 to stop using the data base and software, unlike this case with Horizon. There are over 180,000 out of network providers with Horizon Blue Cross that were short paid.
Horizon has also agreed to remove language that cancelled all assignments of rights by subscribers. Now back in 2009, the current number two person at CMS, Andy Slavitt was the CEO of Ingenix, which is now named Optum Insights. This is who Secretary Burwell feels is who will best serve CMS?
Back in 2009 I was concerned about technology “dupees” being hired at HHS as well, in other words being no contest for the extreme Quant and actuary driven formulas used by insurers for profit an turns out that I was sadly correct and I now refer to it as the Sebelius Syndrome, which also lives in the court systems, in Congress, at the SEC and at the DOJ from time to time. There’s been a lot of discussion about Optum Insights and the United/Optum subsidiary that has been creating the software fixes for insurance exchanges and recently the state of Vermont said they were not aware of the AMA lawsuit when giving QSSI a contract to fix their exchange, and all I can say is there was not much due diligence done there at all, much less a Google search, it’s all out there on the web.
Sadly it’s the same process with Quant generated models most of the time, similar to the AMA lawsuit referenced above where the government gets out foxed with math again and now audits found that insurers for 5-6 years overbilled CMS to the tune of $70 billion, again using complex math models adjusting risk for larger payments. I’m sure just like banks, as was done with the AMA settlement, nobody will have to admit any guilt here on the math model used and CMS doesn’t know what direction to go next on getting the $70 billion back. The link below tells more about this recent audit and it worked for 5-6 years and generated a lot of money on Medicare Advantage claims for insurers. I also seem to think Secretary Burwell understands it all and again former Ingenix CEO Andy Slavitt is now the number two person at CMS answering to Tavenner, who is also in the same boat with not understanding how complex math models work. She recently hired a former Wal-Mart executive to be her legal counsel so I don’t see much action there either, so the work done by the auditors here in finding this automated math model for making $70 billion might go untouched as well and the Sebelius Syndrome might just live on.
Again when most other insurers settled early on, it’s just amazing to find that Horizon was able to hang on to the Ingenix data base and software until this court case was settled and was still being used. It’s the math models that get buried out there, again due to lack of data mechanics logic that we see everywhere today with government getting duped and duped again. The settlement on this was not published until July of 2014 and again one more example of how insurers work complexities to their advantage for profit.
Sadly, this is how the Feds get duped and duped again. Members of Congress have explored the conflict of interest, but again without understanding the complex Quant created and driven math models used by insurers, they are kind of up a creek and really have little impact other than making some noise which is a tiny bit better than nothing. The only Federal agency I’m aware of that’s actually hiring some quants to help them with bank models (same thing quant drive models for profit) is the Office of the Comptroller and it’s at baby stages there as well. Stroll on over to watch some of the videos from folks smarter than me at the Killer Algorithms page , to include quants, to see and understand how all this works, it’s a great learning experience and will make you mad in the process, but it is what it is and is pretty much what keeps inequality acceleration alive in the US for the sake of corporate profits.
So here you have it, years later since the 2009 settlement with the AMA with the data base still being used by Horizon and the sub story of Aetna now trying to weasel out of their settlement proposal. All kinds of legal arguments can be used around math models and code when it comes to judicial cases as such and when the cards are stacked against the government and they don’t  have quants on the other side to assist the lawyers, well we all lose for sure. Just as one other note here, the role of being a doctor too with all of this is hitting hard as well as they too get “scored” with more and more models and that also stands to reduce what they get paid via the use of complex contracts, some even getting paid at rates even less than Medicare.
have quants on the other side to assist the lawyers, well we all lose for sure. Just as one other note here, the role of being a doctor too with all of this is hitting hard as well as they too get “scored” with more and more models and that also stands to reduce what they get paid via the use of complex contracts, some even getting paid at rates even less than Medicare.
You can almost see the frustrations with high level tech folks walking out and quitting the government as it does get frustrating when you have folks “Algo Duped” almost to the point of no return at times, and it’s very scary.
I might guess the levels of frustration were there too with Todd Park, the US CTO, as it’s been reported that he’s going to help get smarter folks recruited for the federal government and that statement itself to me is full-on proof of a smart technologist recognizing the Algo Duping that takes place at high levels of government today. I can barely read or appreciate some of what comes from the White House email bot anymore as again I see the levels of distraction and the stat rat mentality that keeps hurting the real world only seem to grow.
Again I found it amazing that the data base and software was still in use at this point but again right now we have other big issues with “The Grays” in the US to where folks can’t figure out what’s a virtual value and what’s a real world value half the time and we see it all the time with people acting like magpies just repeating stats and numbers all the time, while the real world values get stuffed under the carpet until the real inequality issues erupt again. I don’t know how long our government can continue to function this way with this huge level of distraction but the media is sucked in as well, as all they do is publish meaningless stats to keep everyone distracted. BD
July 14 — Horizon Blue Cross Blue Shield of New Jersey has agreed to amend its out-of-network payment procedures by discontinuing use of an allegedly faulty charging database and providing more transparency for the basis of its payment decisions to its subscribers and health care providers in a settlement approved by a federal judge in New Jersey.
The settlement, which provides no monetary damages to the class members, was approved in an unpublished decision by Judge Stanley R. Chesler on July 9 and settles claims that Horizon violated the Employee Retirement Income Security Act by using the Ingenix database to calculate out-of-network charges.
Eric D. Katz, partner at Mazie Slater Katz & Freeman LLC in Roseland, N.J., told Bloomberg BNA on July 14 that the group of objectors that he represents plans to appeal the court's decision.
According to the court, Horizon has agreed as part of the settlement to discontinue the use of two databases released by Ingenix Inc. as well as a proprietary medical services and supplies charge data profile known as “Top-of-Range” when calculating allowable payments to out-of-network health-care providers.
The insurer has also agreed to revise its health plan language and marketing materials and handbooks to provide a clearer statement of how it derives the allowable payment amounts to out-of-network providers.
“We are pleased that Horizon agreed to discontinue two reimbursement methodologies and make clear in the future the basis of out of network reimbursements to all policy holders,” he told Bloomberg BNA on July 14.
The class members in the instant case alleged that Horizon failed to appropriately reimburse them for out-of-network services they received because it used the “flawed, corrupted and outdated Ingenix" database to determine the UCR for a service
http://www.bna.com/horizons-ingenix-settlement-n17179892313/
 this, but in fact it works! Dr. Mike starts out talking about how a person could help themselves when experiencing a racing heartbeat, or palpitations.
this, but in fact it works! Dr. Mike starts out talking about how a person could help themselves when experiencing a racing heartbeat, or palpitations.  of investing in a human being?’”.
of investing in a human being?’”.  insurer in the face with the allegations of pay for performance measures as it is stated they created an incentive to staff to admit and retain ineligible patients by giving out bonuses and other incentives based up on meeting their targets. It’s also beginning to sound like the same stat rats at the VA as well, who were so stuck on numbers they could not make a left turn to save a life. The bonuses (or as sometimes called P4P) were for staff members who admitted, certified and recertified and discharging patients.
insurer in the face with the allegations of pay for performance measures as it is stated they created an incentive to staff to admit and retain ineligible patients by giving out bonuses and other incentives based up on meeting their targets. It’s also beginning to sound like the same stat rats at the VA as well, who were so stuck on numbers they could not make a left turn to save a life. The bonuses (or as sometimes called P4P) were for staff members who admitted, certified and recertified and discharging patients.  Outreach who’s duty was to troll nursing homes, hospitals and other care facilities to obtain new clients. Now sales portions take place everywhere and nothing wrong with sales people, and they received commissions on the news of new admissions. I can’t see a problem there but as long as the sales calls were good will calls and not looking for ineligible patients.
Outreach who’s duty was to troll nursing homes, hospitals and other care facilities to obtain new clients. Now sales portions take place everywhere and nothing wrong with sales people, and they received commissions on the news of new admissions. I can’t see a problem there but as long as the sales calls were good will calls and not looking for ineligible patients.  at the beginning of 2015 will be a thing of the past. It may not sound like a big deal but for those who are on fixed income, it is a big deal that helps. Again this applies towards those who retired before 2000 as those who retired later already had their subsidiary ripped. BD
at the beginning of 2015 will be a thing of the past. It may not sound like a big deal but for those who are on fixed income, it is a big deal that helps. Again this applies towards those who retired before 2000 as those who retired later already had their subsidiary ripped. BD  and maybe something unexpected popped up in that area as the note does reference the hospital wants to be a “safe” facility. In addition the hospital has also had financial issues in struggling to pay both employees and vendors in the last 3-4 years. Who knows, maybe they need a loan to fix the boiler? RKM Management is the owner of the hospital. The ER room is closed and the next closest facility is 24 miles away which concerns residents.
and maybe something unexpected popped up in that area as the note does reference the hospital wants to be a “safe” facility. In addition the hospital has also had financial issues in struggling to pay both employees and vendors in the last 3-4 years. Who knows, maybe they need a loan to fix the boiler? RKM Management is the owner of the hospital. The ER room is closed and the next closest facility is 24 miles away which concerns residents.  and thus there’s the tug and pull and if it is subsidiary of an insurance company, there’s a lot of a revenue stream with the audits.
and thus there’s the tug and pull and if it is subsidiary of an insurance company, there’s a lot of a revenue stream with the audits.  decisions and I would imagine there could be quite a few takers on this as it represents one less headache of bean counters in the virtual/real world confusion we live in today which I call “The Grays”, a very big problem indeed.
decisions and I would imagine there could be quite a few takers on this as it represents one less headache of bean counters in the virtual/real world confusion we live in today which I call “The Grays”, a very big problem indeed.  This is a new project that is measuring the use of orthopedic or prosthetic devices and the patient owns the device and the data, very cool. The
This is a new project that is measuring the use of orthopedic or prosthetic devices and the patient owns the device and the data, very cool. The  Why? We all know insurers make a ton of money selling our data and they buy a lot of our data as well. Here’s an example of a company that buys your credit card data, analyzes it and “scores” your behavior before selling it as then they can charge the insurers more and of course this comes out down the tubes in higher premiums at some point as all of this is not cheap as companies are making millions doing this. So staying away from data selling entities like this are a sure win for consumers here.
Why? We all know insurers make a ton of money selling our data and they buy a lot of our data as well. Here’s an example of a company that buys your credit card data, analyzes it and “scores” your behavior before selling it as then they can charge the insurers more and of course this comes out down the tubes in higher premiums at some point as all of this is not cheap as companies are making millions doing this. So staying away from data selling entities like this are a sure win for consumers here. 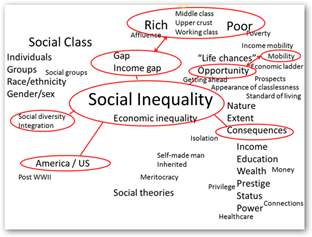 We license people for things with far less risk, like a license to catch a fish for one example, sell real estate, sell stock, do hair and nails and the list goes on and there’s nowhere near the big risk is with selling data as the consumers get hurt. Licensing would not stop data selling but it would rather make companies accountable and transparent, as the levels of flawed data are on the rise out there too.
We license people for things with far less risk, like a license to catch a fish for one example, sell real estate, sell stock, do hair and nails and the list goes on and there’s nowhere near the big risk is with selling data as the consumers get hurt. Licensing would not stop data selling but it would rather make companies accountable and transparent, as the levels of flawed data are on the rise out there too. 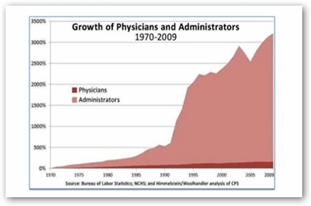 I also said when this situation first erupted that this was the issue with the administrators at the VA living too much in the virtual world. If you happened to watch one report from Anderson Cooper, he commented and walked away with the same perception “all they talked about were their numbers”. So again a report like this is not going to be completely conclusive and maybe it’s the news media tweaking the title here a bit too?
I also said when this situation first erupted that this was the issue with the administrators at the VA living too much in the virtual world. If you happened to watch one report from Anderson Cooper, he commented and walked away with the same perception “all they talked about were their numbers”. So again a report like this is not going to be completely conclusive and maybe it’s the news media tweaking the title here a bit too?  a lot of that out there and I write about it all the time. Again being I was a developer and partly due to the way I’m wired I can pick it like a sore thumb.
a lot of that out there and I write about it all the time. Again being I was a developer and partly due to the way I’m wired I can pick it like a sore thumb.  know in tech that to help those not in tech we have to change our terminology into some form of “Pig Latin” so others can understand what’s going on, what needs to be done, etc. In other words, translate from tech world to the layman world and that’s not always easy to do. There are some that lie and cheat during this process and they eventually are found out when someone else gets a glimpse of their code or just flat out calls “foul”. The White House privacy person quit as well and she may have been the wrong person in the wrong job from what I saw from her short term in office too.
know in tech that to help those not in tech we have to change our terminology into some form of “Pig Latin” so others can understand what’s going on, what needs to be done, etc. In other words, translate from tech world to the layman world and that’s not always easy to do. There are some that lie and cheat during this process and they eventually are found out when someone else gets a glimpse of their code or just flat out calls “foul”. The White House privacy person quit as well and she may have been the wrong person in the wrong job from what I saw from her short term in office too.  but it it necessary and you don’t have to write code to have it, but it is easier to master if you have written code. Just last week every one in technology just laughed our asses off listening to the new White House Cyber Security Head just brag about how he has very little technology background. Well we all know he’s headed down the delusional perception path and he’s up to be a big “dupee” for sure. Just the fact that he made that speech tells you he’s going to to be a dupee.
but it it necessary and you don’t have to write code to have it, but it is easier to master if you have written code. Just last week every one in technology just laughed our asses off listening to the new White House Cyber Security Head just brag about how he has very little technology background. Well we all know he’s headed down the delusional perception path and he’s up to be a big “dupee” for sure. Just the fact that he made that speech tells you he’s going to to be a dupee. 
 What’s even scarier sometimes is to listen to them talk about their own perceptions at times too.
What’s even scarier sometimes is to listen to them talk about their own perceptions at times too.  which they are entitled to do by all means. Sure it got the attention of some California lawmakers but if they don’t do it in public they can still contact the lawmakers without a public display.
which they are entitled to do by all means. Sure it got the attention of some California lawmakers but if they don’t do it in public they can still contact the lawmakers without a public display.  I do like the content here too that Tech Dirt brought up about our next
I do like the content here too that Tech Dirt brought up about our next  r so that explains the politics here as it’s never easy for them, but his claims were important as he exposed serious problems with the transplant record keeping and they fired him afterwards. The battle then went forward with Dr. Steve Goldschmid, dean of the UA College of Medicine.
r so that explains the politics here as it’s never easy for them, but his claims were important as he exposed serious problems with the transplant record keeping and they fired him afterwards. The battle then went forward with Dr. Steve Goldschmid, dean of the UA College of Medicine. 
 he can’t see his doctor anymore as they don’t see any Covered California patients. That is frustrating and this might go back to the mess with doctors getting paid 30% less from Blue Cross and Blue Shield with policies bought through the exchange. It was so bad for a while that the insurers had to go back and up the reimbursement a bit and still the lists of who was in network and who was not was still a mess.
he can’t see his doctor anymore as they don’t see any Covered California patients. That is frustrating and this might go back to the mess with doctors getting paid 30% less from Blue Cross and Blue Shield with policies bought through the exchange. It was so bad for a while that the insurers had to go back and up the reimbursement a bit and still the lists of who was in network and who was not was still a mess.  Blue Shield showed that we were discounted some 20-30% of our previously paid services and the check was now going to the patient and not the provider. We have been trying to get these checks from the patients who love getting these Blue Shield checks and keeping them. As physicians are finding this out they are mad and are starting to demand payment up front from the patient and give them a superbill so they can bill Blue Shield. What a mess.”
Blue Shield showed that we were discounted some 20-30% of our previously paid services and the check was now going to the patient and not the provider. We have been trying to get these checks from the patients who love getting these Blue Shield checks and keeping them. As physicians are finding this out they are mad and are starting to demand payment up front from the patient and give them a superbill so they can bill Blue Shield. What a mess.” part of the settlement here, not to use it anymore. The big AMA court case filed by Cuomo in New York was for 15 years of short paying doctors all across the country. It was not just United/Optum involved here as they licensed it to other insurers, like Aetna who proposed their case at the end of last year for underpaying for around 15 years. Health Net if I remember correctly was one of the first to stop using the data base and settle.
part of the settlement here, not to use it anymore. The big AMA court case filed by Cuomo in New York was for 15 years of short paying doctors all across the country. It was not just United/Optum involved here as they licensed it to other insurers, like Aetna who proposed their case at the end of last year for underpaying for around 15 years. Health Net if I remember correctly was one of the first to stop using the data base and settle.  to those who saw the doctor’s body. He had just completed his residency at NYU and he left his keys and NYU ID on the roof.
to those who saw the doctor’s body. He had just completed his residency at NYU and he left his keys and NYU ID on the roof.  about how it was impacting folks in Tennessee and you can see in the video and comments that consumers were by algorithmic error being sent to the wrong kind of doctors as a replacement, i.e. gynecologists as their new family practice MD and more.
about how it was impacting folks in Tennessee and you can see in the video and comments that consumers were by algorithmic error being sent to the wrong kind of doctors as a replacement, i.e. gynecologists as their new family practice MD and more.  a hospital outside of New Jersey.
a hospital outside of New Jersey.