Once again the drive and race for data is on the move, insurers will fall over themselves 10 times over to get a hold of data to analyze. I agree with the comments from the Komen Foundation, an insurance company should not be doing this type of evaluation, it’s easy to be a Monday morning quarterback when you are not the doctor and the patient and looking at statistics only. They live and die by all the numbers and with their numbers relative to breast cancer, look at what they do when it comes to testing for the Breast Cancer hereditary gene. Even if they do allow it, it is all kinds of red tape for both the patient and doctor.
The Genomic Test for BRACAnalysis (Breast Cancer) To Be Scrutinized by United Health Care
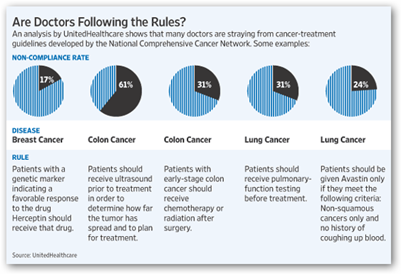
Below is the chart they made up to show how many are and are not following the “rules”. I have conducted interviews on this blog with companies that have technologies and procedures that can either save lives or dramatically improve the quality of life and they complain that it takes an insurance company sometimes years before they will approve the treatment, and many of these items are not high cost cancer treatments either.
It’s back to what decision making algorithms they choose to run. We are back again to compliance in the breast cancer area and granted therapy given in an office is easy to trace compliance as the patient is there for the treatment, but their numbers show a large number of non compliant patients with medications. There are many assistance program out there that help get the drugs for free or almost free and you can bet this was not taken into account with the numbers, the IPAs never get this right either.
You can’t ever be 100% here, but the way it is written it seems like the doctors are not talking enough about side effects, which I find to be a bit of a stretched analysis with some bean counter sitting on one too many beans, but when they speak of compliance they will hold to these numbers exactly and pound the doctor for compliance, has gone on for years with insurance companies. This is the same thing that happens all throughout the company with employees, the algorithms that produce the decision making processes don’t leave enough room for flexibility, and thus we see some real stupid stuff in the press. The level of elevation and press attention that has to be met at times is what really turns everyone off.
I might speculate here that Roche may not be too happy with United questioning the use of Avastin either, granted it is costly and perhaps some cost improvement could be seen in the future here, but we are stuck at the point where money rules with these folks and the human side of healthcare is long forgotten. I realize studies offer information and have value, but the one of the biggest problems is the entire way the insurance industry operates: their attitude. 
In healthcare, you can’t use cost to justify every decision as we are humans and some along the line seem to have forgotten this fact. BD
UnitedHealthcare, a unit of the nation's largest health insurer based on revenues, has started sending doctors individualized reports assessing their treatment of breast, lung and colorectal cancer patients. The reports show that while breast-cancer patients generally receive care that conforms to professional protocols, treatments given for colorectal and lung cancer tend to fail to meet expert recommendations more often.
Cancer is United Healthcare's third-most-expensive disease, at a cost of $2.5 billion a year, after cardiovascular disease and orthopedic joint procedures. The company says its goal is not to rank or reward medical practitioners. Rather, it hopes that drawing doctors' attention to how their treatments might vary from medical protocol will reduce unnecessary care that doesn't improve health and raises health-care costs.
Some critics say that monitoring quality is not the appropriate role for an insurer, which has a financial interest in all this. "This is one area I'd rather have doctors police themselves than have an insurance company do it," says Eric Winer, chief scientific adviser for Susan G. Komen for the Cure, a research and educational organization.
The company especially probed the use of high-price biotech drugs, which it says it found in some cases are being prescribed inappropriately. One NCCN guideline for colon-cancer patients advises that patients get chemotherapy after surgery, but in 31% of cases, the care did not comply with the rule. Instead, in the bulk of those cases, patients were prescribed Avastin, a Roche Holding AG biologic that is unproven in that patient group, says Dr. Newcomer. And among patients with non-small-cell lung cancer, about 24% received Avastin, even though their disease didn't meet the right criteria to get the drug, UnitedHealthcare found.
UnitedHealthcare also looked at whether breast-cancer patients were compliant with their medication. It found that 38% weren't filling prescriptions for their aromatase inhibitors, drugs that stop the estrogen production that can feed certain cancers. Knowing that their patients are non-compliant can prompt doctors to talk with the patient about whether side effects are bothering them, the company said.
UnitedHeath Group Sends Reports Assessing Doctors' Treatment - WSJ.com



0 comments :
Post a Comment