This is a great article and in the New York Times today and it has been broken down to show the overall mathematics that are used to determine payments. We are again, back to the “A” word that you see plastered in the center of this blog, an algorithm. I just finished watching a PBS documentary called “Facing Death” and clearly up front too in this video the doctor states that to make life saving decisions, they are relying on the algorithms to help them make decisions as it is complicated, as we have so many more alternatives and things that can be done to save a life and when to use which methodologies to have an improved outcome is complicated. We are all still humans and we can predict everything as miracles still exist today and to deprive one of a potential miracle is something nobody wants to live with when making decisions as such.
As far as what hospitals get paid, this is a huge topic and it is discussed on the web almost every day and payments do vary from one hospital to the next in the same area and in different states. You almost have to read up on being a bit of an economist to completely comprehend the calculated formulas, aka algorithms. Some state legislatures are coming of age with wanting accountability with private insurance algorithms, like in New Jersey.
New Jersey Legislature Getting Smart– Bill to Modify Claim Procedures to Include Asking For Insurance Company Algorithms-Bill A3334
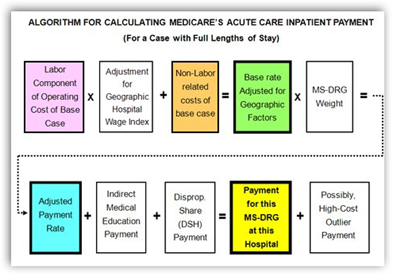
The article further goes on to say that the pricing too does not seem to indicate better quality but is rather driven by market value, in other words the contracts that are negotiated today. The payment systems are supposed to be transparent, which in essence they are to a degree, that is if you are an economist and understand the algorithmic formulas, but most of us don’t unless you sit down to fully study the entire situation and the author here has done a good summary of explaining in layman’s terms what this means. All the medical coding that everyone complains about enters into this arena for the government to make their assessments. How else do you think they know how many cases of pneumonia for example are diagnosed every year. Those codes, known as an ICD9 are the key to compiling those statistics.
Labor charges are calculated and they are summarized to a degree as they vary from one facility to another. If you go back to a case of pneumonia that is complicated with diabetes, then the outcome and projection will change as now you have 2 health situations to formulate. Hospitals that see uninsured patients get a higher level to help compensate and then there is also the break they receive on taxes if they are non profit. Again without a full study time on your part, it takes a while to get to the absolute understanding.
Further more the author makes a comparison here to private health care insurance and the fact that it is not transparent, in other words we do not get to see their algorithms and how they calculate which is something I make a point of here quite frequently. Also worth noting too is the fact that the algorithms calculated by Medicare are largely created by information that is provided by health insurance companies who are Medicare contractors, so the relationship of Medicare data and private insurance is tight, in other words they have the data. This leads to stories in the news of people being turned down for care when private insurers use their algorithms to project and determine eligibility and claim payments. Unlike Medicare they run algorithms to determine what money they will need to pay under a risk category and as Wendell Potter has explained to us many times, Wall Street sees any claim payment made as loss when you look at profit and investor standpoints, and it does make one wonder why do we support such a system? There reaches a time when the algorithms used do not support ethics and outcome. Two years ago I started suggesting that we need a Department of Algorithms or something along this line.
“Department of Algorithms – Do We Need One of These to Regulate Upcoming Laws?
We all currently hate the complicated systems we work with today for profit and it’s not getting any better with contracts, so if a system were created with private insurers that set pricing standards, it would certainly make life easier all the way around and we can all certainly deal with a little less marketing. Have you had a conversation with either a hospitalist or ER doctor lately to hear about the decision making algorithms they use for payment in order to first of all get the best care, and secondly adhere to their goals of keeping the price down? If not, ask one and you might get an earful if they like talking. Many may not want to talk about it and I can’t blame them as they are stretched out beyond ethics at times and again there’s the constant pressure of the hospital to keep costs down from the administrative side as doctors as a whole are going to do what they do best to save a life. Private insurers are up to their ears in lawsuits with the use of cost cutting formulas.
Insurance Companies Under Attack with Lawsuits – Generated by Their Algorithms
So in summary a simpler system with algorithms that are less complicated would certainly be something that would be welcome I feel as again when care is needed with so many differentiations of treatments available and the pricing that is added every day due to new technologies and treatments available, it would certainly stand to reduce some stress all the way around when it comes down to who is going to pay what and to who. BD
In a previous post, I described how Medicare came to adopt price schedules for hospitals and physicians that are now derided as Soviet in origin. Actually, as I noted, this was a home-grown American idea that Presidents Ronald Reagan and George H.W. Bush embraced and introduced to Medicare.
In this and the next post I would like to describe how this system works, starting with inpatient hospital services. I will draw on the excellent literature provided by Medpac, the independent Medicare Payment Advisory Commission established in 1997 by Congress to advise it on issues affecting the Medicare program.
Medicare’s payment system does have an underlying rationale that can be explained to market participants. It is fully transparent. And it does strive for horizontal equity, meaning that it pays hospitals in similar situations the same price for the same service.
Although this system can and does accommodate adjustments for local market conditions and sometimes even rewards what policy makers value – extra payments for services provided to underserved areas – it is primarily cost-based rather than value-based, which I and other policy analysts would prefer.



0 comments :
Post a Comment