Just a few months ago I wrote about the Cray YarcData that CMS is using to search for and detect fraud that is running a MarkLogic data base and search agent. MarkLogic began as a search engine app and grew into a data base program. You may have heard the company name with the news that went around about the Healthcare.Gov website. In this capacity with the utility the mission here is to detect patterns and look for fraud.
Cray Computers Making a Big Comeback Thanks to Big Data–CMS Using Cray YarcData Unit To Detect Fraud Patterns With Payments
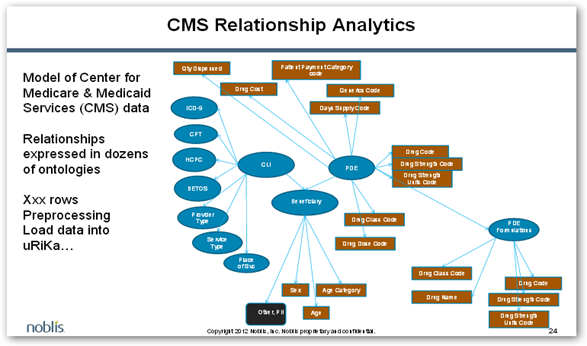
Below is an image that shoes the CMS data relationships, so again with having this capability writing new search parameters would yield a lot of information if this the course they choose. This is still pretty new and where they go searching looking for fraud patterns.
Again the review here with data parameters would require a human effort as well as false positives will be in there as well with results when you query large data resources like Medicare. The claim information queries can tell a lot with checking an MD’s NPI number against being registered, etc. I’m not sure how they would really enforce that as some doctors who are not registered with Medicare might occasionally write a prescription when filling in for another doctor who is in Medicare and is the primary physician.
Right now the article says the Medicare Fraud investigators can’t access data, well they can buy prescription data like everything else from Milliman or Optum/Ingenix if they wanted to as those two have been selling prescription data for years to everyone else out there, or they can buy it from the AMA who buys from both of these companies. Prescription data does not fall under HIPAA. Access remotely to the Cray appliance would give some searching capabilities to the fraud investigators as well. If the data mining is done correctly at CMS and not taken out of context to identify the real abusers, which of course is a small group of the entire medical community then they should be able to find those few doctors that lead to the abuse of prescription drugs.
They are taking comments and the entire pdf can be read here. BD
Medicare plans to arm itself with broad new powers to better control — and potentially bar — doctors engaged in fraudulent or harmful prescribing, following a series of articles detailing lax oversight in its drug program.
The Centers for Medicare and Medicaid Services described the effort Monday in what's known as a , the standard process by which federal agencies make significant changes.
Two of the changes mark a dramatic departure for the agency, which historically has given much higher priority to making medications easily accessible to seniors and the disabled than to weeding out dangerous providers of health care.
For the first time, the agency would have the authority to kick out physicians and other providers who engage in abusive prescribing. It could also take such action if providers' licenses have been suspended or revoked by state regulators or if they were restricted from prescribing painkillers and other controlled substances
Under the rule change, the contractor would be given the power to access the records directly. The inspector general of the Department of Health and Human Services has repeatedly pressed Medicare to make this change.
And the agency will tighten a loophole that has allowed doctors to prescribe to patients in the drug program, known as , even when they were not officially enrolled with Medicare. Under the new rules, doctors and other providers must formally enroll if they want to write prescriptions to the 36 million people with Part D coverage. This would require them to verify their credentials and disclose professional discipline and criminal history.



0 comments :
Post a Comment