I believe everyone probably remembers when this test first became available for women to see if they would have a genetic background that would see if they had a risk for developing breast/ovarian cancer. As time moves forward we now have additional information and the insurers are analyzing the women and the information they are receiving from such tests. Humana and Aetna are also looking at the requests received for the test.
Originally when the test came out, it was certainly viewed as valuable and still is, but the question lies on who really needs the test, again with additional information collected and recent reports on questionable over treatment of breast cancer in some areas.
Marketing of the test is now being questioned along with being sure that women are actually getting the correct and enough decisive information to impact treatment decisions. Myriad, the company with the rights to the test of course still wants to maintain market share of providing the test and there have been a couple recent challenges in this area too with other companies wanting to participate and not have proprietary set of algorithms done just at one company. Again, as in much of healthcare as technology and research moves forward, we are looking at potential change here, and the company of course is looking to keep the testing process as is so as not to lose revenue.
The Genomic Test for BRACAnalysis (Breast Cancer) To Be Scrutinized by United Health Care
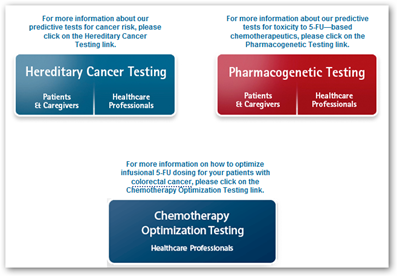
I think the questioning here of the test somewhat shows how genomics is evolving with the additional information we are getting and more so how it interfaces with patient care. We talk about being overloaded with information today, and the field of genomics is no exception in the amount of data the processes that are run to get to the core information we are looking for to work our way into better personalized medicine. As you can see from the diagram below, it’s not one simple test but has 3 different focuses. BD
Several insurers have instated prior authorization, prior notification, and mandatory genetic counseling procedures prior to covering Myriad's BRACAnalysis test to ensure that the test is being given to the right patients.
Data from two national insurers, Humana and Aetna, shows that around 20 percent of requests for the test do not meet requirements for BRCA testing under their policy. A United Healthcare official has cited competitors' data suggesting that as much as 80 percent of requests for Myriad's BRCA test are withdrawn after pre-certification and genetic counseling procedures are conducted.
According to Sue Friedman, executive director of the patient advocacy group Facing Our Risk of Cancer Empowered, a growing number of breast and ovarian cancer patients are reporting instances of receiving either too little or the wrong information about their genetic risk for developing cancer from commercial firms




0 comments :
Post a Comment