As we all know or should know by now the claims are all pretty much electronically processed whether one is going direct or if using a clearinghouse. Even if an office 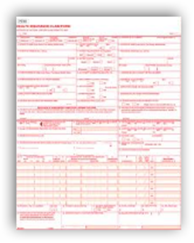 is still all paper, chances are they are using a billing service who submits either direct or via a clearinghouse. If the physicians stated that the condition will not improve then it gets kicked over to a denial or discontinue section and this all comes back to a degree of coding for this to occur.
is still all paper, chances are they are using a billing service who submits either direct or via a clearinghouse. If the physicians stated that the condition will not improve then it gets kicked over to a denial or discontinue section and this all comes back to a degree of coding for this to occur.
This is sometimes where hospitals and physicians accidentally get into trouble with trying to code for the patient care. Some that know the process a little better than others may have figured out how to work around some of this and I’m not saying it is correct or wrong as you can’t without seeing each claim and patient condition. In this case cited the coverage for skilled nursing was discontinued for the purpose of it not being able to show improvement. Again, claims go through the coding and processing mills and if this is the outcome, then usually the customer service folks read out to you what is on the screen along with the designated text that corresponds to the code. If the claim cannot be elevated to a second consideration and perhaps resubmitted with more appropriate codes if applicable, then in the “denial” frame work it sits with the same results on the screen.
Also, one does not want to code illegally either and make sure all appropriate modifier codes are in place too and sometimes those modifiers make all the difference in the world on whether or not a claim is approved and paid, so again was it the coding or is is the built in algorithm that came into play here with these 2 cases? At any rate a court case is needed to appeal the decision of one algorithm that discontinued coverage for both patients and perhaps be the subject of a review. In 5 weeks the file did not indicate improvements to allow coverage for subsequent bills, so away went the coverage.
See why everybody hates coding in the medical business, it’s a bitch! BD
WASHINGTON — Two federal courts have ruled that the Obama administration is using overly strict standards to determine whether older Americans are entitled to Medicare coverage of skilled nursing home care and home health care.
Medicare will pay for those services if they are needed to maintain a person’s ability to perform routine activities of daily living or to prevent deterioration of the person’s condition, the courts said. Medicare beneficiaries do not have to prove that their condition will improve, as the government sometimes contends, the courts said
After hip replacement surgery, Ms. Papciak received skilled nursing care, physical therapy and occupational therapy in a nursing home. Medicare terminated coverage after five weeks, saying her condition had not improved and was unlikely to improve.
Medicare Coverage Standards Are Too Strict, Courts Find - NYTimes.com



0 comments :
Post a Comment