I like this answer as the AMA is of course stating they are pleased with the options and opportunities, but they are also real in this statement. It’s confusing, tough and  a lot of information to read through and practices will have a lot of questions and will need “Health IT” support (let’s not forget this involves billing) to get set up on the initiatives and it could even go beyond this level I would guess with maybe even getting to the point of helping the doctors with their discussions with the hospitals.
a lot of information to read through and practices will have a lot of questions and will need “Health IT” support (let’s not forget this involves billing) to get set up on the initiatives and it could even go beyond this level I would guess with maybe even getting to the point of helping the doctors with their discussions with the hospitals.
CMS Created Four Bundled Plans for Payment and Is Looking for Hospitals and Physicians to Participate
In case you missed it a couple weeks ago a report is out that states it costs doctors a ton of money already annually to keep up with the insurer red tap so add this to till? By the time all the bills are paid, here in southern California, I have a few former MD clients that don’t even clear 100k a month for themselves! When I spoke at the e-MDs annual meeting I spoke with a clinic that had each doctor working from 8 am to 8 pm and seeing over 100 patients a day! They weren’t complaining but trying to figure out how to further automate and gee that is getting harder to do! Remember these practices still need to see patients as it is still the people business and the small practices are not just small data silos that see patients on the side.
Health Insurance Paper Work Costs Doctors an Average of $83k a Year
Now if that isn’t enough, listen up and read here on the CIO side of things and how the ICD-10 is the straw that is ready to break the camel’s back.
Dr. Halamka Speaks About Health IT–“CIOs are on Overload” and It Would be A Blessing to Stall Off ICD-10 to 2016 - The Straw Breaking the Camel’s Back
This is a good statement as we have so many in positions that are making these  timeline and data decisions, who don’t do any of this themselves!! Get a clue soon, please! Non participant executives who don’t understand Health IT and data flows are killing us as they don’t get it and have absolutely “no hands on” experience to help them in this area.
timeline and data decisions, who don’t do any of this themselves!! Get a clue soon, please! Non participant executives who don’t understand Health IT and data flows are killing us as they don’t get it and have absolutely “no hands on” experience to help them in this area.
They can’t debug themselves!!
Meaningful Use-Money And Data Being Thrown Every Which Way To See What Sticks With Limited Expertise And Not Enough Time at the Top to Lead a Full Debugging Process
Shoot CMS this is still the people business and look at how you want everyone to find the time do all of this. Consumers have just pretty much shunned it as they want to spend all the time to learn and only get involved in tracking down information when a claim is denied. We don’t even have an active REC center in Orange 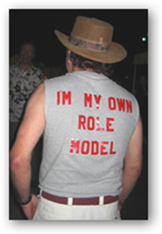 County, California either, and I guess they got the money but zero has been done and their information page is still part of the over all Cal-Optima Medicaid insurance site as that’s who received the contract.
County, California either, and I guess they got the money but zero has been done and their information page is still part of the over all Cal-Optima Medicaid insurance site as that’s who received the contract.
Does our Surgeon General get involved here as she would be a good one having her great background with doctors and patients before her appointment, as she battled this stuff but I’m guessing she’s on overload right now too. How about this from a year ago with improving Health literacy? I hear nothing from anyone being a role model and working with all of this data and billing themselves, so how in the world do they know what the real work load is, they don’t. I have blogged about our lack of role models for over 2 years now and we still get these timelines and additional red tape sent the way of both doctors and patients from the “non participants” that have no clue.
HHS National Plan to Improve Health Literacy – Not Going To Happen Until We Focus on Using Technology (The Tool for Literacy) Which Includes Role Models at HHS And Other Places in Government
Again, nice statement from the AMA with being realistic here and putting the cards on the table right up front, help the practices and do more than just put out information on websites, as that’s about all we see right now with some pretty unattainable standards. due dates, and wishes being put forth. BD
Immediate Past-President, American Medical Association
"The American Medical Association (AMA) appreciates CMS' responsiveness to our interest in bundled payments. We are pleased the initiative provides flexibility and a range of models. This may be an important opportunity to learn how to organize these approaches to improve patient care, quality, cost of care, and practice economics.
"We look forward to reviewing the details of the application criteria, and we urge CMS to encourage applications for physician-led bundling initiatives. We urge CMS to be prepared to provide technical assistance and data to interested physicians who may not have experience with bundled payment models."



0 comments :
Post a Comment