Ok we are now starting to see some of the 3rd party risk companies used by insurers being questioned. When they make their sales pitch to insurers they of 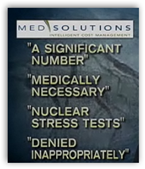 course tell them how much money they can save them, a percentage usually. The video talks about approval for tests and what is allowed and what is not allowed.
course tell them how much money they can save them, a percentage usually. The video talks about approval for tests and what is allowed and what is not allowed.
What controls these cost evaluations – those algorithms!
In this case a nuclear stress test was ordered by his doctor and it was denied by Blue Cross 3 times and the doctors had to go to work and interesting how this video shows a web conversation with him and his doctor too. After 3 times the doctor sent the patient to the hospital where a big blockage was found and if he had not received treatment he would dead said the doctor at the hospital. He had an emergency quadruple bypass.
Visit msnbc.com for breaking news, world news, and news about the economy
Med solutions is the 3rd party who worked for Blue Cross promising 25-30% savings, they run algorithms to do this based on data input into the system and the patient records they have on file. Med Solutions ended up with a Senate investigation and found that sure there were some denied appropriately but how about the ones inappropriately denied, like in this case. If your life is on the line it’s one huge difference and 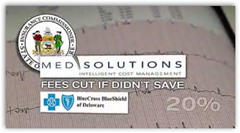 someone better fix that algorithm. Med Solutions fees were to be cut if it didn’t save Blue Cross 20% with their auditing, so you can think about what may have gone on here. Back in 2007 I found an old post here with a doctor complaining about Aetna and Med Solutions getting grilled in a peer to peer meeting as it did not meet the criteria set forth.
someone better fix that algorithm. Med Solutions fees were to be cut if it didn’t save Blue Cross 20% with their auditing, so you can think about what may have gone on here. Back in 2007 I found an old post here with a doctor complaining about Aetna and Med Solutions getting grilled in a peer to peer meeting as it did not meet the criteria set forth.
“Because the test I ordered did not fit Aetna’s or Medsolution’s “protocol”, quite possibly created by businessmen without much medical background, my patient must suffer. I should not need to provide justification for preferring to perform one study over another as long as each is appropriately ordered.”
Who’s playing doctor here? Their argument was that they want to guarantee that patients get the care they need, well maybe if you not looking at having your rates cut. Interesting too is that I tried to visit the Med Solutions website today and it is down, which could be coincidental but maybe not. Blue Cross changed their  procedures and said they no longer require approval for nuclear stress tests. This was good case that made it to the news for an awareness for all and perhaps they will look closer at the algorithms run by the 3rd party software folks they used in the future.
procedures and said they no longer require approval for nuclear stress tests. This was good case that made it to the news for an awareness for all and perhaps they will look closer at the algorithms run by the 3rd party software folks they used in the future.
Now do you see where our lawmakers are having issues here with quick changes in algorithms like this when patients are denied care. The link below is a long post and covers a lot of territory about digital illiteracy in lawmaking and why some processes should change and I included a video from Harry Markopolos to remind us of the fact that we can’t take dull knives to gun battles.
Healthcare Reform Law– Is Any Judge Fully Capable of A Decision on a Law That is Challenged By Constantly Changing Algorithms?
We certify software from medical record vendors, so why do we not certify that he algorithms run by insurers and their agents are also performing correctly?
We need some digital algorithms on file to save time and patients like this the anguish. I wrote this back in 2009 by the way on the Department of Algorithms. BD
“Department of Algorithms – Do We Need One of These to Regulate Upcoming Laws?
msnbc video: Health insurers putting squeeze on tests



sometimes the problem is as simple as the billing person or office help not submitting the claim correctly.add to that, the "third party..software solutions" program might not have invested any time or trouble contacting the physician to have the claim corrected, if it was improperly coded or submitted, in some way? the communication disappears, the claim gets rejected when, in fact, it might have been "saved" from being "lost" if the 2 parties had discussed the proper submission.
ReplyDeleteHave I seen this happen? ,,hehe..why do you ask?
Med solutions denies every request without fail. On one occasion they did approve, only to send a letter the next day to say it wasn't approved.
ReplyDeleteFlorida branch of MedSolutions called 2 days before a scheduled appointment for an MRI to "reschedule with an in-network provider" was told would save a significant amount on cost... they then referred to a much more expensive lab & changed authorizations on existing appointment. Original lab was in network but MedSolutions claimed not to even be able to find their info.
ReplyDeleteRequired several hours of phone calls to original MRI provider, the lab that they attempted to schedule with and Aetna to get straightened out and original appointment restored. FL MedSolutions office then stopped answering the phone in the middle of a weekday & had to call MedSolutions home office. Even though MedSolutions *are* contracted with Aetna, they or some part of their FL affiliate are clearly involved in some shady business. If you do get authorized & already have an appointment with an in network provider, save yourself the chaos and refuse to allow them to change it!