Who do you want to make decisions about your healthcare? Physicians are driven to care by financially incentivized with folks who are not involved in direct healthcare. The first video is a contains highlights from this day’s events addressing “Taking Back Medicine”. Who’s giving all the private groups all the power to determine if physicians are good doctors. The American Board Internal Medicine Board makes around $41 million dollars a year having doctors taking certification and maintenance of license tests. Dr. John Tedeschi is a family practice doctor in New Jersey and this conference was held on “Doctor’s Day” this year.
Mentioned in the presentations given is the Hippocratic oath and if you have never heard of it, it’s an oath to do no harm taken by every doctor. 
“The oath has been modified multiple times. One of the most significant revisions was first drafted in 1948 by the World Medical Association. Called the Declaration of Geneva, it was "intended to be a self-conscious rewriting of the Hippocratic Oath, reaffirming Hippocratism in the face of the shame and tragedy of the German medical experience"
“It’s time for internists, family practices, surgeons, etc. to come together. As physicians, we are continually told what to do by business administrators and financial organizations,” states Dr. Tedeschi. “Sacrificing human lives should not be used to save an economy and is not the American way”. He further goes on to talk about nurse practitioners being put in place to replace what doctors provide for care. Sure there’s a time and place for nurse practitioners I say but not to replace doctors entirely but it seems like there’s a big push in this direction. I recently made a blog post about the CMS is ready to remove CME (continuing medical education) in open payments as the agency fears they could be giving the impression of endorsing corporate sponsorship. I didn’t realize until reading some of the material out on the web how this connects to the ACA (Affordable Care Act) with medical boards and their processes.
The video below is a condensed version of the highlights of the “Doctor’s Day” conference, and if you would like to watch the full hour long presentation you can go here. The American Board of American Specialties requires all doctors to maintain their certification. Dr. Tedeschi states these are corporations running certification processes. Maintenance of certification is required to maintain reimbursement from Medicare and Medicaid and this was modified by the Affordable Care Act which changed Social Security Laws. States are looking to replace licensing, which is MOL (Maintenance of Licensing) with MOC (Maintenance of Certification) which is run by the American Board of American Specialties, so it’s the ABAS who stands to profit in a big way.
Now let’s dig in a little bit here and courtesy of Cardiologist Dr. Wes we have some legal and other implications of the Maintenance of Certification that has been added to the Affordable Care Act, as you can read in reference number one below. In the law and ACA it now stipulates that unless doctors are certified, they cannot be reimbursed by Medicare and Medicaid. There are many doctors practicing currently who are not certified, who have never been certified who see Medicare and Medicaid patients. Emergency room doctors, is perhaps another question with certification. It’s a bit complex as is everything today to understand the full impact.
The Effects of Maintenance of Certification and Crony Capitalism
This note was recently posted on Sermo
"I just got results from recent ABIM 10 yr recert and I failed. I over prepared for this exam, studied daily for months, Harvard review course, analyzed over 1000 board type questions the week before, teach medical students daily. I have never come close to failing any previous board exams."After a panicked e-mail was sent to the American Board of Internal Medicine (ABIM) inquiring if there might be an error in the scoring of the examination, this email was received:
Dear Dr. B:
Thank you for your recent e-mail to the American Board of Internal Medicine (ABIM).
ABIM is entirely satisfied that there was no error in scoring your examination. The scoring process is a meticulous one. A rigorous set of quality control steps are carried out on every examination. Before final scores are approved, the reliability, validity, and fairness of the examinations are verified by the ABIM. ABIM will not release results until it is satisfied that a reliable instrument has been administered and data are accurate. Additional information about the way ABIM develops and scores its examinations is at ABIM's website at www.abim.org/about/examInfo/developed.aspx.
If you would like to have your examination rescored, please put your request in writing. All requests must be received within six months of the results' mailing date. Include your name, candidate identification number, the examination to be rescored, and a check for $250.00 payable to the American Board of Internal Medicine. Send to:
Rescore Request
American Board of Internal Medicine
510 Walnut Street, Suite 1700
Philadelphia, PA 19106-3699
Results of the rescore will be mailed to you within eight weeks of receiving your request.
If you need further assistance, you may reply to this e-mail or call us at 1-(800)-441-ABIM (2246) Monday through Friday, 8:30 a.m. to 8:00 p.m., and Saturday, 9:00 a.m. to 12:00 p.m. EST.
Respectfully,
Ethan Lambert
Customer Service Representative
American Board of Internal Medicine
510 Walnut Street, Suite 1700
Philadelphia, PA 19106
Phone: 1-800-441-ABIM
215-446-3500
Fax: 215-446-3590
www.abim.org
This scenario could happen to any US physician undergoing the American Board of Medical Specialties (ABMS) proprietary Maintenance of Certification program today. The hundreds of hours of preparation, survey collection, and timed test, all wasted. And since hospital credentials, legal credibility, and inclusion on insurance panels are increasingly requiring a favorable certification "status," the potential consequences to U.S. physicians are very serious indeed.
This threat to U.S. physicians' ability to practice medicine comes at a time when insured patient populations have swollen. So why would such a "Maintenance of Certification" program be beneficial for American's? Is such a program really about assuring some definition of quality physician? Or might it be about something very different?
While the realities of this situation are sure to raise physician emotions (and maybe the concerns of patients, too), there are several important facts that all physicians and interested patients should understand regarding the American board of Medical Specialties' (ABMS) Maintenance of Certification process that is administered by the American Board of Internal Medicine (ABIM):
- The Patient Protection and Affordable Care Act (Affordable Care Act)1 modified sections of Social Security Law2 to require Maintenance of Certification of physicians as a condition of receiving payments from Centers for Medicare and Medicaid Services (CMS).3
- While other organizations may create a "qualified Maintenance of Certification program," the only program specifically authorized in the Affordable Care Act is the Maintenance of Certification program from the American Board of Medical Specialties (ABMS).3
- "Qualified Maintenance of Certification" programs must contain surveys as part of their criteria4 despite their lack of scientific rigor.
- According to law, the Maintenance of Certification program will be operated by a "specialty body" of the American Board of Medical Specialties" that meets the criteria for a registry or physician quality and efficiency measurement" for physician payment. It is now clear this "specialty body" is the American Board of Internal Medicine (ABIM).3
- CMS will receive a portion of $5 million dollars in 2014 from the Federal Hospital Insurance Trust Fund and $15 million from the Federal Supplementary Medical Insurance Trust Fund for the first 6 months of 2015. The National Quality Forum also receives a potion of these funds5
- The Administrator of the CMS shall through contracts develop quality and efficiency measures (as determined appropriate by the Administrator) (editor's note: along with "multi-stakeholder group input into selection of quality and efficiency measures")6
- The current President and CEO of the American Board of Internal Medicine, Richard J. Baron, MD served as Chair of the ABIM Board of Directors in 2008 and as Treasurer of the Board in 2007 and later as a Trustee for the ABIM Foundation while also serving as the Group Director, Seamless Care Models, at the Innovation Center at CMS.
- The former President and CEO of the American Board of Internal Medicine, Christine Cassels, MD, left the ABIM to join the National Quality Forum, another "consensus-based entity," and also had significant conflicts of interest with the group purchasing and performance improvement firm Premier, Inc and Kaiser Foundation Health Plans and Hospitals which she later relinquished. Despite these conflicts, she retains her current position.
- An unfinished public webpage (Here's a backup screenshot in case this webpage disappears) raises speculation that current ABIM President and CEO, Richard J. Baron, MD might be slated to sit (or may currently sit) on the National Quality Forum's Board.
Crony capitalism is pervasive in Washington, DC and nowhere is this more evident than the American Board of Medical Specialties and the American Board of Internal Medicine incorporation into our new health care law. The conflicts of interest contained within the Affordable Care Act's requirement of Maintenance of Certification as a basis to assess physician quality are increasingly harmful to physicians. Given the conflicts of interest between the American Board of Internal Medicine, National Quality Forum, and the Center for Medicare and Medicaid Services, paired with the growing Maintenance of Certification failure rates of physicians without a clear explanation, the specter of cost control at the expense of patient care must be considered.
Only by understanding the environment of government cronyism and regulatory entrapment created by our new health care law can physicians begin to address these very real concerns for patient care.
-Wes
References:
1 Full text of Affordable Care Act: (pdf 2.1 MBytes)
2 42 U.S. Code § 1395w–4 - Payment for physicians’ services
3 ACA law pdf above, page 247 (124 STAT. 365)
4 ACA law pdf above, page 845 (124 STAT. 963)
5 42 U.S. Code § 1395aaa - Contract with a consensus-based entity regarding performance measurement
6 42 U.S. Code § 1395aaa-1 - Quality and efficiency measurement
My own addition here is referencing item number 6 mentioned and it states the “CMS Administrator” through contracts will develop efficiency measures so let me add that the number two person at CMS as an administrator came right from Optum/United Healthcare again is who’s contracted here to set these policies? It’s a good question is it not? 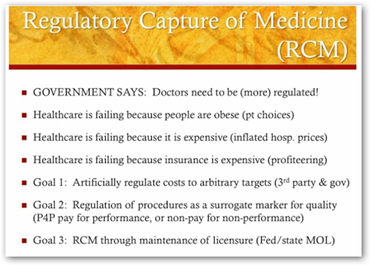 We all know Tavenner with just a background in nursing by trade is not competent to set such standards that apply to doctors; and in the creation of of the ACA, not one doctor was included. It sounds like it’s back to corporations again running doctors with their analytics. I remember myself asking the question back in 2009 if Kathleen Sebelius and Nancy Deparle had the business intelligence to model the ACA law, which were the two primary individuals held accountable. I realize with such a big project like the ACA that sure there were some things modeled which would need addressing or amending and this looks like another item as there has been many.
We all know Tavenner with just a background in nursing by trade is not competent to set such standards that apply to doctors; and in the creation of of the ACA, not one doctor was included. It sounds like it’s back to corporations again running doctors with their analytics. I remember myself asking the question back in 2009 if Kathleen Sebelius and Nancy Deparle had the business intelligence to model the ACA law, which were the two primary individuals held accountable. I realize with such a big project like the ACA that sure there were some things modeled which would need addressing or amending and this looks like another item as there has been many.
Payers run a very complex world of algorithmic formulas and that’s part of the profiteering that goes on there and in other places in healthcare. Like I said above my worry back in 2009 was about the government having people in place that were educated and ready to deal with it intelligently and sadly not as we can see the number of events that have fallen into place not only here but look at the SEC for another glaring example with people at the top that have no clue on how computer code works and functions. IT infrastructures are running everything today.
In addition we are seeing many of the models fail today as healthcare is the people business and yes I understand looking at cost and useful analytics by all means but the models are not working as they were designed. I read years of Lewin reports that stated billions and even a couple with Trillions mentioned would be saved, and guess what, that has not happened. What has happened is that we are spending money big time on Health IT and software grows on itself. In my opinion, there are not any “experts” left as algorithmic scoring and formulas have turned most into “nickel economists” with “ideas” that may or may not work.
Healthcare Policy Experts/Politicians - They Really No Longer Exist and Consumers Are Too Busy Being Chased by Algorithms Anymore to Care About You Anyway…
We need doctors and everyone talks of shortages of them, so why are we making it so hard for them to function? We all are experiencing complexities in life and the rush on doctors is even more so. The “coding” portion of a doctor’s job today is not popular with any doctor. I just finished reading that from 2010 to 2012 the number of MOC's applied for dropped from over 7000 to about 1500, and is still falling. We also have a lawsuit filed now from the AAPS.
The Association of American Physicians & Surgeons (AAPS) has filed suit April 23, 2013 in federal court against the American Board of Medical Specialties (ABMS) for restraining trade and causing a reduction in access by patients to their physicians. The ABMS has entered into agreements with 24 other corporations to impose enormous “recertification” burdens on physicians, which are not justified by any significant improvements in patient care.”
MOC (Maintenance of Certification) and MOL (Maintenance of Licensing) are the two names used back and forth on this process. Some states are working towards or have over ridden the process of not bringing in MOC to replace MOL. Here’s another video below talking about how MOC and MOL conflicts with normal CME(continuing education) that doctors have used for years. Dr. Robert S Maurer states there are 38 organizations that can come in to a medical practice, fine a doctor, or send one to jail where there used to be four and that’s scary in itself.
Today I was reading a marketing article saying that providers now may have the opportunity to earn extra money if they cut down wait times within standards set by insurance companies. Now I don’t know any doctor that is not trying to get patients in as if they are not seeing patients then they are not making any money, right? Of course that is correct but I saw all kind of consumers retweeting this information..wake up folks as this is just one more what could be called quantitated justification for nixing performance and paying less. You were “had” on that one if you took it in as something that was going to improve the performance of doctors.
I mention that above as doctors have so many quality numbers coming at them and targets, one insurance company has their numbers and another insurer has a different set, so if a doctor is taking several insurance plans, well multiply that out. Besides that on the hospital side we have CMS that has not woken up yet and still thinks we need a “5 Star Rating Program” for hospitals, when in fact with many closing or changing services and contracts with doctor groups, we just want to know who’s going to be left and where we “can” go, that’s the real world.
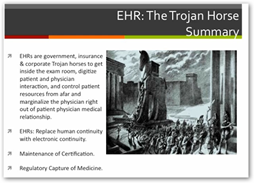
Here’s a presentation on the medical record Trojan horse by Dr. Craig Wax. Again he’s talking about how it works for doctors and the stimulus money and a view from how a practice looks at it. We know of course that electronic medical records are here to stay, but what kind, how complex and where did the doctors get left out? I wrote an early medical records program and it was for the doctors but now payers are involved and made the entire process very complex and they are making money by doing this. Money in coding and documentation is over ruling good healthcare.
Dr. Wax talks about the carrot and the stick with the government in his presentation and risk assessments and all the electronic tools they need to have today. Sure we are not going back to paper by any means but the processes can use some work and be simplified. The ONC office of HHS is almost to the point to where they can’t answer some of the questions posed to them as well as far as the certification processes for medical records, as their jobs with figuring out what processes need to be in place for medical record certification. As I always tell everyone, software builds on itself and that’s a prime example there with trying set the standards with a complex world of medical software that is changing daily. When things get too complicated people give up and we don’t want doctors to give up as most of this is a technology war with trying to have the right parts of it in the right place.
If you are not a doctor, this is interesting to watch to get a view from the other side from Dr. Wax. Now with claims settlements, insurers can go back in and deduct something that was paid three years ago when folks begin looking at data. When data ages and a claim is no longer fresh we come back to “context” and if you read here enough I talk about that all the time with people taking data and applying various modes of focus or contest to a point they are trying to show. Scroll on down to the footer of this blog and watch video #1 for more about how that works and how” numbers don’t lie but people do.”
Listen to Dr. Wax discuss how the complexities work and then we get into the big data side of all of this. Again keep in mind you are hearing this doctor speak as it affect his life and his business as we only hear mostly about the patient side, which is important too but just listen to see how all of the Health IT expenses and risk assessments affects a primary doctor.
Dr. Wax did another presentation you might want to watch here with his view on the government’s role with healthcare today.
I’m asked quite frequently “what’s wrong with doctors”..it’s not the doctors it’s the models. We all know that both insurance and stock markets both like complexities as that means profits. I think we are seeing a lot of “doctor scoring” here, same thing that we as consumers and patients are subjected to. I like good data and information that makes me smarter but in my own observations we are trying to push way too many “Bloomberg Big Gulp” models that don’t work in healthcare. As the link below says…people don’t work that way.
People Don’t Work That Way” A World of Broken Software Models That Don’t Align To the Human Side,Too Much Push At Times With Only A Proof of Concept That Fails in the Real World..
Look at this image comparing the growth of administrators to physicians to the right, look at the number of administrators to keep of those doctors.
In summary we have the “scoring of doctors” just as the World Forum on Privacy reported on the “Scoring of America” 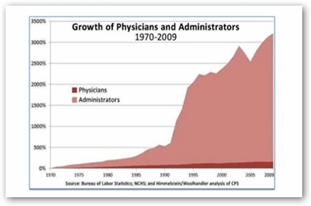 here to where based on analytics, which we don’t know if they are correct or not, denies, care, money, etc. So is the MOC and MOL necessary? The current CME model is working and not failing and a doctor has to be responsible of course to maintain this. Are the boards just making money with more “scoring” than what is really required?
here to where based on analytics, which we don’t know if they are correct or not, denies, care, money, etc. So is the MOC and MOL necessary? The current CME model is working and not failing and a doctor has to be responsible of course to maintain this. Are the boards just making money with more “scoring” than what is really required?
Sure we need some levels of checking and balance too but has this gone too far and with the government involvement and the too big to fail insurance company involvement and is this where it’s coming from? We like good models and I understand keeping costs down but all the analytics out there are not saving money and quality of care in the US is falling. A couple years ago I said that half of the analytics purchased would be a waste of money anyway as it’s more about making money and selling data as insurers make a lot of money doing that and companies like Walgreens make $1-2 billion a year selling data.
I should also close here with the fact that once a doctor does get certified and “scored”, there will be more data to sell and believe me that is part of the profit process here as listed of the MOC process, doctor data will go up for sale with all types of information relative to the process of this certification and that’s part of the money making process. We have already seen this from the patient side being abused with the ability to buy a list of people infected with HIV for one example. MOC processes via the American Board of American Specialties will have their data to sell as well so let’s not forget this side of the entire issue that goes along with then entire package as data selling and scoring consumers in the US is an epidemic in the US as noted by the World Forum on Privacy.
The True Dangers With Corporate Obsessive Algorithmic Scoring of US Consumers - It Creates More Flawed Data For Sale And Makes Banks and Companies Wealthier As the Pace of Inequality Accelerates …
If you are a consumer or a doctor reading this, one more word to the wise when looking up information about doctors, please avoid Healthgrades and Vitals websites if you want accurate information as you won’t be finding it there as these sites are horribly flawed with the data they provide about doctors and hospitals. The sites make money on ad exposure and is just one more area in healthcare data that is not what it appears to be. Both sites state they use state board information but how often do they update or how often are the state boards updating is the questions that always arise with flawed data like this online. BD
If you like to see the full version of the conference use the link below…



0 comments :
Post a Comment