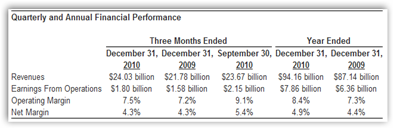
Below are some of the highlights from the press release you can read in it’s entirety  at the link at the bottom of the post. Profits were up from last year which came in at $1.58 Billion and basically people were not going to the doctor was one of the reasons cited for additional income this year. We all know how healthcare reform has been nothing so far profits for carriers no matter how loud they complain. Premium dollars grew with additional policies and less could afford to do to the doctor.
at the link at the bottom of the post. Profits were up from last year which came in at $1.58 Billion and basically people were not going to the doctor was one of the reasons cited for additional income this year. We all know how healthcare reform has been nothing so far profits for carriers no matter how loud they complain. Premium dollars grew with additional policies and less could afford to do to the doctor.
“Algo Profits Were Up”
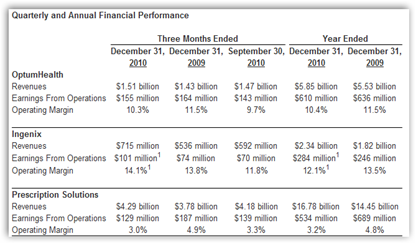
The “algorithm” side of their business, Ingenix and subsidiaries increased 10% and if you watched the news this year there were more then plenty  acquisitions made at the tech level of the company, subsidiary watch. When you look at the sector of business below on the chart, prescription and health revenue units were down but the algorithm revenue was up! There’s money in those Algos.
acquisitions made at the tech level of the company, subsidiary watch. When you look at the sector of business below on the chart, prescription and health revenue units were down but the algorithm revenue was up! There’s money in those Algos.
Ingenix (algorithm) revenue increased to $2.3 billion, 28% over the year. These services are sold as technology and some use their services for anti fraud auditing, but least we forget the 15 year Ingenix case of over charging and the refunds issued to doctors and patients, so again it’s always good to know where the mathematical formulas point these days. Ingenix got out of the property casualty medical business this year with the sale of one of their subsidiaries.
Here’s an example of a United/Ingenix contract via acquisition earlier this year with the VA now doing business with a United subsidiary.
VA Awards Contract to Picis, Subsidiary of Ingenix for Anesthesia Record Keeping Software
It may be too soon also to see how the China investment is moving along as it also falls under the algorithm part of the business. You have to go 3 layers down the daisy chain of subsidiaries to find this one. It does get confusing today with all the mergers and acquisitions to really put your thumb on who is doing what, when and how at times as when data gets merged for accelerated data intelligence, waters get cloudy. I3, a company owned by Minnetonka-based  UnitedHealth's technology arm.
UnitedHealth's technology arm.
UnitedHealth subsidiary (Ingenix Subsidiary I3) Acquires ChinaGate – Working to Sell Chinese Products Globally
From the website:
“We are familiar with the Chinese regulatory system and are well connected with most of the top urban class A hospitals and clinical trial centers that are GCP certified by the China State Food and Drug Administration (SFDA). Moreover, since we worked many years in multi-national pharmaceutical companies ,we are well versed in ICH, European and United States Food and Drug Administration (FDA) requirements on Good Clinical Practice (GCP). “
With combing data and reaching out for business there were also expenditures for programs created like putting pharmacists on pay for performance at Walgreens to sign individuals up for various programs and some of the data for this mining exercise was to be created via the Ingenix data end of United to programmatically predict who was going to be a patient with selected chronic conditions.
You can read more about Ingenix MedPoint here.There’s also a flash presentation where you can view the process here. Here’s a little more detail on how the costing algorithms work by doing a risk assessment based on getting information on your medications from drugs stores and pharmacy benefit managers.
“By increasing understanding of potential disease conditions and relative risk, MedPoint enables underwriters to more accurately project future claims costs on a case-by-case basis.”
The company also made a splash at CES this year in joining in as a platinum sponsor which shows a somewhat varied business plan for marketing than what we have seen in the past.
Going to CES This Year? Healthcare Represented With Mobile Devices and Insurance Companies-United Healthcare A Sponsor This Year
In addition United owns a bank with over a billion on deposit for health savings  accounts under its Optum Health group and if you read the news this year loans were made to many healthcare agencies through the Optum Financial Services. division.
accounts under its Optum Health group and if you read the news this year loans were made to many healthcare agencies through the Optum Financial Services. division.
UnitedHealth Group Owns a Bank With Deposits Surpassing a Billion – OptumHealth Bank FDIC Insured
Long and short of it is that mergers and acquisition of technology divisions make it possible to run the rest of their business through the creation and modification of business models using algorithms and code to predict and project business intelligence and profit directions. In addition, with all the mergers and acquisitions occurring, we don’t know what next levels of data will be collected and analyzed yet for the next areas of profit making to be explored. That takes time and some of the acquisitions are still fairly new so it may take the algorithm folks at Ingenix a while to figure out a plan as to how to approach and maximize the data to achieve even higher levels of profits next time around.
In the meantime, as citizens we are basically left with having to take a knife to a gun battle when it comes to getting our care and battling claims as years of data has been collected, and all of it is not always correct, but it is held against the consumer in so many ways with a data rap sheet that is dumped on the consumer to prove incorrect if needed.
Companies in the health insurance business crank up the Algos and create a  report in a minute and consumers spend months and years to correct data that we had nothing to do with the input and profits for such algorithms continue to make for huge profits on Wall Street. Sadly to say the very same methodologies are graduating in format to healthcare too.
report in a minute and consumers spend months and years to correct data that we had nothing to do with the input and profits for such algorithms continue to make for huge profits on Wall Street. Sadly to say the very same methodologies are graduating in format to healthcare too.
High Frequency Electronic Trading Methodologies And Algorithms Work Their Way Into Healthcare With Human Bodies Losing Liquidity With the “Data Game”
“It is a technological arms race in financial markets and the regulators are a bit caught unaware of how quickly the technology has evolved”
Full Year Revenues of $94.2 Billion Increased 8% Year-Over-Year, and Include a 10% Increase in Fourth Quarter Revenues to $24 Billion
Health Services Revenues Reached $25 Billion in 2010, up 15% Year-Over-Year
Health Benefits Businesses Served 1.2 Million More People in 2010, Including Growth of 230,000 People in Fourth Quarter
MINNEAPOLIS--(BUSINESS WIRE)--UnitedHealth Group (NYSE:UNH) today reported fourth quarter and full year 2010 financial results, including strong revenue growth from both its Health Benefits and Health Services business platforms. Full year and fourth quarter 2010 net earnings were $4.10 per share and $0.94 per share, respectively.
Stephen J. Hemsley, president and chief executive officer of UnitedHealth Group, said, “Our strong advances in serving customers across key performance measures over the past two years have come from a consistent focus on fundamental execution. That focus is driving growth and favorable business results. We are positive about the future and our potential to address evolving market needs. We believe our two primary platforms – Health Benefits and Health Services – will be effective vehicles for deploying our assets and resources to help address the broad needs of customers and key participants in the health system and health care marketplace.”
Management anticipates UnitedHealth Group’s 2011 revenues will approximate $100 billion, based on strong customer retention and new growth across its businesses, as well as contributions from recent acquisitions. The Company affirmed its outlook for 2011 net earnings in the range of $3.50 to $3.70 per share.
UnitedHealthcare Community & State, Ingenix and Prescription Solutions – increased revenues by more than 10 percent year-over-year in both the full year and the fourth quarter
UnitedHealth Group Reports 2010 Results, Highlighted by Strong Growth | Business Wire



0 comments :
Post a Comment