Well first of all there was the news that Dr. DeSalvo has left the ONC for a better job at HHS as Acting Assistant Secretary of Health and I have to say she might be a lot happier there as being a doctor, he knowledge and skills are right in there with working on tackling Ebola. So far none of the MD ONC directors have lasted that long and in fairness, I think it’s a tough job as a doctor to come in and head up a Health IT operation and regulation department. Maybe that’s why they don’t stay too long. Myself and others have asked that question a few times but it looks like this was a good stepping stone for her to move up to her new position. They have lost quite a few folks of late at the ONC and right now it’s a tough place to be with the complexities the ONC is facing with updating Meaningful Use regulations and rules. We have had a lot of changes for stage two and the AMA sent in their shopping list as well on what they recommend.
good stepping stone for her to move up to her new position. They have lost quite a few folks of late at the ONC and right now it’s a tough place to be with the complexities the ONC is facing with updating Meaningful Use regulations and rules. We have had a lot of changes for stage two and the AMA sent in their shopping list as well on what they recommend.
Update: I also read where Dr. Jacob Reider, Deputy Director of the ONC is leaving at the end of November.
Next up on the list is this new “Clinical Practices Initiative” and you can read the press release below. I don’t know how many doctors are going time for yet another program as such and the idea of course sounds great as far as communicating but some of the MDs I am hearing from today are saying when they are done with Meaningful Use two, that’s it, they’re done with the government. Of course they still have quality stats and so forth that are required but anything extra to add on right now gets really hard. Some doctors who have been in Meaningful Use since the start have already thrown in the towel and moved on since the bonus money gets smaller at the end and the complexities along with running their practice are just more than they want to fit in. It all depends where they are at in the program I think and what their schedules look like.
I see this as being yet something for doctors to do and the time their office spend with claims and insurance companies has risen as well and just by their nature most doctors kind of collaborate anyway within their own circles. Again I’m in the real world and sometimes folks in government agencies become a little too virtual with what they think the real world can do when establishing goals and overshoot. CMS has been under that gun for a while now and they have relied on a lot of mentoring from United Healthcare for a number of years. A couple of former CMS folks told me that, need a number fix, go ask United. Furthermore look who’s gone to work at the ONC and CMS, former United Healthcare employees. We all know that Andy Slavitt who is the number two person at CMS right now was the CEO of Ingenix when the AMA sued them in a class action suit a few years ago and now we have a United Healthcare lawyer heading up privacy at the ONC, so coming from a huge data selling insurer, I’m not holding my breath there as HHS/CMS/ONC decide to “lawyer up”.
ONC Hires New Privacy Head, A California Corporate Lawyer From United Healthcare, One of The Biggest Operating Data Selling Companies In the US
Right now most are not happy with Obamacare or the ACA which ever you want to call it as it’s just a bunch of broken algorithms that don’t work together and we have insurers who are hiring quants by the groves and remodeling the plans they offer right and left. That was my big concern back in 2009 with Sebelius being a big duper and she did get duped as she’s no contest to the very smart math modelers insurers use. 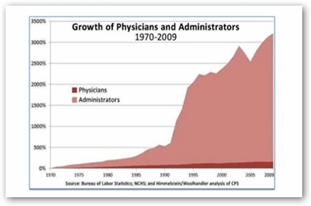
Data Scientists/Quants in the Health Insurance Business–Modeling Beyond the Speed and Capabilities of Humans To Keep Up With The Affordable Care Act–Turning Into A World of Killer Algorithms That We All Hate..
When you look at all the doctors being fired as Medicare Advantage providers from United, it’s all algorithms and doctors have told me it’s nuts as they are putting together doctors that have never worked together before. Also it’s getting harder with contract for consumers to find both a doctor and a hospital covered by the same insurer too, again models used by insurers that use numbers and stats don’t take that into account and just low cost routing, along with what other parameters they put in there. Where I am at, many doctors work for big physicians groups that are owned by United Healthcare and their complex contracts they sign to be in network, nets them reimbursements at levels less than Medicare. You can give the image a look and see the number of doctors out there compared to administrators, a bit shocking if nothing else.
Again I just think some of the government agencies spent too much living in virtual worlds and that’s a problem all over when folks are confused and cant’ tell the difference between virtual world values and the real world. We have hospitals shutting down, running out of money all across the US and the entire HHS/CMS group is oblivious to this it seems, just get those stats in here so we can rate you:) I learn a lot from Quants as well and this is what they tell me “People don’t work that way” and they build models and the good ones don’t get lost in virtual values only. Even the White House puts out numbers that nobody can predict and actually it makes them look bad.
People Don’t Work That Way” A World of Broken Software Models That Don’t Align To the Human Side,Too Much Push At Times With Only A Proof of Concept That Fails in the Real World.
Here’s the part that bothers me is that they are pulling numbers out of the sky as nobody can predict this as there’s items out there called “variables’ so here we go with fake numbers to get you all stirred up and who knows if they are going to try and put this in their budget too. This is some quantitated madness here and better looked at in 4 years rather than try to project this now. Again we have some algo duping going on here. If you read the news of late, the Mayor of Chicago came up short with his projected numbers on cameras catching speeders, about $50 million and he put it in his budget. The mayor of Chicago by the way is the former Chief of Staff at the White House, so pretty typical duping there with one lost in the virtual world.
“HHS officials think this initiative can prevent 5 million unnecessary hospital admissions over the next four years, and reduce health care costs by at least $1 billion.”
To save a billion this is way too much hassle for doctors to mess with in my opinion as again doctors collaborate anyway and are adults and do know when they need to do that. After all doctors live and work in the “real” world so I guess you could say this big brainstorm would be typical of those who spend their time in virtual worlds more than the real world, as their perceptions get so out of whack with what we read and see at times. BD
FOR IMMEDIATE RELEASE
October 23, 2014
Contact: HHS Press Office
202-690-6343
HHS Secretary announces $840 million initiative to improve patient care and lower costs
New initiative will support networks that help doctors access information and improve health outcomes
Health and Human Services Secretary Sylvia M. Burwell today announced an initiative that will fund successful applicants who work directly with medical providers to rethink and redesign their practices, moving from systems driven by quantity of care to ones focused on patients’ health outcomes, and coordinated health care systems. These applicants could include group practices, health care systems, medical provider associations and others. This effort will help clinicians develop strategies to share, adapt and further improve the quality of care they provide, while holding down costs. Strategies could include:
Giving doctors better access to patient information, such as information on prescription drug use to help patients take their medications properly;
Expanding the number of ways patients are able communicate with the team of clinicians taking care of them;
Improving the coordination of patient care by primary care providers, specialists, and the broader medical community; and
Using electronic health records on a daily basis to examine data on quality and efficiency.
“The administration is partnering with clinicians to find better ways to deliver care, pay providers and distribute information to improve the quality of care we receive and spend our nation’s dollars more wisely,” said Secretary Burwell. “We all have a stake in achieving these goals and delivering for patients, providers and taxpayers alike.”
Through the Transforming Clinical Practice Initiative, HHS will invest $840 million over the next four years to support 150,000 clinicians. With a combination of incentives, tools, and information, the initiative will encourage doctors to team with their peers and others to move from volume-driven systems to value-based, patient-centered, and coordinated health care services. Successful applicants will demonstrate the ability to achieve progress toward measurable goals, such as improving clinical outcomes, reducing unnecessary testing, achieving cost savings and avoiding unnecessary hospitalizations.
The initiative is one part of a strategy advanced by the Affordable Care Act to strengthen the quality of patient care and spend health care dollars more wisely. For example, the Affordable Care Act has helped reduce hospital readmissions in Medicare by nearly 10 percent between 2007 and 2013 – translating into 150,000 fewer readmissions – and quality improvements have resulted in saving 15,000 lives and $4 billion in health spending during 2011 and 2012.
Building upon successful models and programs, such as the Quality Improvement Organization Program, Partnership for Patients with Hospital Engagement Networks, and Accountable Care Organizations, the initiative provides opportunities for participating clinicians to collaborate and disseminate information. Through a multi-pronged approach to technical assistance, it will identify existing health care delivery models that work and rapidly spread these models to other health care providers and clinicians.
“This model will support and build partnerships with doctors and other clinicians across the country to provide better care to their patients. Clinicians want to spend time with their patients, coordinate care, and improve patient outcomes, and the Centers for Medicare & Medicaid Services wants to be a collaborative partner helping clinicians achieve those goals and spread best practices across the nation,” said Patrick Conway, M.D., deputy administrator for innovation and quality and CMS chief medical officer.
Practice Transformation Networks. CMS will award cooperative agreements to group practices, health care systems, and others that join together to serve as trusted partners in providing clinician practices with quality improvement expertise, best practices, coaching and assistance. These practices have successfully achieved measurable improvements in care by implementing electronic health records, coordinating among patients and their families, and performing timely monitoring and interventions of high-risk patients to prevent unnecessary hospitalization and readmissions. Practice Transformation Networks will work with a diverse range of practices, including those in rural communities and those that provide care for the medically underserved.
Support and Alignment Networks. CMS will award cooperative agreements to networks formed by medical professional associations and others who would align their memberships, communication channels, continuing medical education credits and other work to support the Practice Transformation Networks and clinician practices. These Support and Alignment Networks would create an infrastructure to help identify evidence-based practices and policies and disseminate them nationwide, in a scalable, sustainable approach to improved care delivery.
By participating in the initiative, practices will be able to receive the technical assistance and peer-level support they need to deliver care in a patient-centric and efficient manner, which is increasingly being demanded by health care payers and purchasers as part of a transformed care delivery system. Participating clinicians will thus be better positioned for success in the health care market of the future - one that rewards value and outcomes rather than volume.
HHS encourages all interested clinicians to participate in this initiative. For more information on the Transforming Clinical Practice Initiative, please visit: http://innovation.cms.gov/initiatives/Transforming-Clinical-Practices/



0 comments :
Post a Comment