One of the most valuable additions will be adding “business intelligence” those  algorithms that analyze and help create reports and find fraud. As we all know patching only goes so far and then it’s time for the entire remake. This is probably way over due as the prior administration in processing claims for Medicare outsourced all of this to insurance companies as you see today with contractors either being direct or subsidiaries of insurance companies that run to make a profit. Recently the Office of Personnel Management wants to create their own data base to learn about the reporting functionality needed too.
algorithms that analyze and help create reports and find fraud. As we all know patching only goes so far and then it’s time for the entire remake. This is probably way over due as the prior administration in processing claims for Medicare outsourced all of this to insurance companies as you see today with contractors either being direct or subsidiaries of insurance companies that run to make a profit. Recently the Office of Personnel Management wants to create their own data base to learn about the reporting functionality needed too.
Office of Personnel Management Data Base Wants to Learn  How to Create Those Cost Savings Algorithms Too-Analyzing Government Employee Private Plans
How to Create Those Cost Savings Algorithms Too-Analyzing Government Employee Private Plans
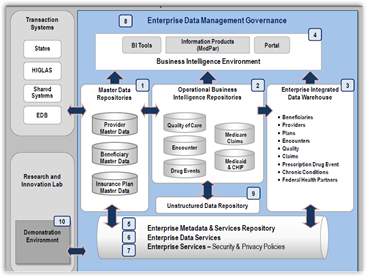
“The data in the EDE exists in raw form, and does not reveal the trends and comparisons that CMS needs to make mission-critical decisions. To meet these and other vital data access needs, CMS is implementing an enterprise-wide  Business Intelligence Environment (BIE) that provides essential operational analytics and reports—the front-end query, advanced analytics, and reporting solutions—that will help CMS use its data to inform important decisions and offer greater confidence in those decisions.”
Business Intelligence Environment (BIE) that provides essential operational analytics and reports—the front-end query, advanced analytics, and reporting solutions—that will help CMS use its data to inform important decisions and offer greater confidence in those decisions.”
We have folks in Congress that still bear down on HHS over why enough fraud is not being fought and again this comes back around to knowing what insurance subsidiaries are up to – Subsidiary Watch as this has changed a lot in the last 2 years and the 70s are long gone. The link below gives some enlightenment there with everything having been outsourced that CMS doesn’t really have a complete infrastructure and contractors have to motivation to fight fraud as the other side of their business collected those profitable transaction fees so they are not going to cut too many of those and transaction fees pay both on good claims and those that are fraud, again knowing what the other subsidiary has going on today and who they partner with too. BD
YOU HAVE TO KNOW THIS STUFF AS IT STANDS TODAY.
Medicare Fraud Prevention Has Cases Falling Through the Cracks–Looks Who’s Getting the Contracts And Check Out the Algorithms For Their Profitable Business Models
The project is slated to being in the first quarter of 2011. You can read the full report here in pdf format, it’s a lot of pages.
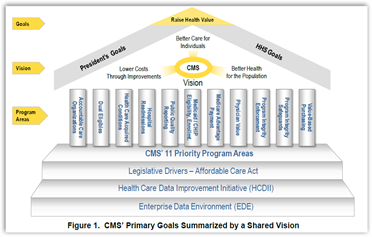
WASHINGTON – The Centers for Medicare and Medicaid Services, the largest healthcare payer in the country, has released a plan for upgrading its computer and data systems with the aim of providing better care. The Patient Protection and Affordable Care Act mandates the overhaul.
The Centers for Medicare & Medicaid Services (CMS) provides healthcare services to approximately 100 million beneficiaries and pays benefits totaling approximately $800 billion a year.
The law calls for a modernized computer system that makes data available "in a reliable and timely manner to providers of services and suppliers to support their efforts to better manage and coordinate care furnished to beneficiaries of Medicare programs" and supports "consistent evaluations of payment and the delivery system reforms under CMS programs."
CMS plan details upcoming computer upgrades | Healthcare IT News



0 comments :
Post a Comment