The average layman is normally not aware of all the processes and transaction charges that are coupled with processing a medical claim. This is a huge profit area with algorithmic formulas that are sold to companies in the business of processing  claims in healthcare. As we all have read, Ingenix and United Healthcare have been busy buying up a lot of these services this last year. We all know what a claim denial costs as far as time and effort to appeal and so forth. Let’s just look at one aspect of the process. The company below held value as Ingenix, the wholly owned subsidiary of United paid over a billion to obtain these data processes that audit and help predict denials before they happen. The link below was from July of 2010 and there are some additional subsidiaries mentioned as well.
claims in healthcare. As we all have read, Ingenix and United Healthcare have been busy buying up a lot of these services this last year. We all know what a claim denial costs as far as time and effort to appeal and so forth. Let’s just look at one aspect of the process. The company below held value as Ingenix, the wholly owned subsidiary of United paid over a billion to obtain these data processes that audit and help predict denials before they happen. The link below was from July of 2010 and there are some additional subsidiaries mentioned as well.
UnitedHealthGroup On The Move to Potentially Purchase Executive Health Resources for Around 1.5 Billion – Too Big To Fail or Is It Too Big to Insure?
Each transaction for accessing services from a data base normally has an associated charge and this is where the big money is made with algorithmic formulas that check and balance claims and use what is called business intelligence to project risk at times too. I have said this business feeds itself and here’s one example of this type of process. In addition to having a claim denial, one can now purchase additional transaction type services to be able to predict what claims will be denied and again more than likely this is one more transaction fee that is added on for someone, usually the submitter to pay for in this process. Again there’s some financial value here as I don’t think United would have shelled out over a billion to purchase this company if not. In short with one of the services they offer there’s now a new algorithmic formula to handle the denial process for  submitters before it gets denied. The question comes about of something like “do we need this service and will the additional transaction fees we pay show a return on investment”. If this is determined then additional transaction fees are added if a purchase of services is made normally, thus adding to the complexity of processing medical claims and the cost.
submitters before it gets denied. The question comes about of something like “do we need this service and will the additional transaction fees we pay show a return on investment”. If this is determined then additional transaction fees are added if a purchase of services is made normally, thus adding to the complexity of processing medical claims and the cost.
Why do we see all these algorithmic based companies flourishing we might ask? As the process for getting paid and predictive modeling continues to grow, so does the software/algorithmic processes available to handle and the price. Gee as a patient or doctor, one probably has no clue as to how much IT services and queries are being run on one single claim! To do this of course the company has to maintain extensive information on all the nationwide payors and needs to collect and aggregate all this data to submit their approach for a solution. In addition they also sell this algorithmic service to do the same for ![]() Medicare and Medicaid medical claims and handle appeals, so once more when purchasing such, is there value here and is the expense on the process going to save time and be worth the investment of moving it outside?
Medicare and Medicaid medical claims and handle appeals, so once more when purchasing such, is there value here and is the expense on the process going to save time and be worth the investment of moving it outside?
Case managers are given a portal to connect with and the web based tools to use  and there are a number of auditing companies they connect with as well who provide their workflow/data management solutions so you can get an idea here of how many of these algorithmic services they aggregate and represent, all to check and audit that medical claim and assure you upfront as best they can that it won’t be denied or has inaccurate information. For most reading here these are companies you more than likely have never heard of, but again it’s the algorithmic monitoring and transaction fee based
and there are a number of auditing companies they connect with as well who provide their workflow/data management solutions so you can get an idea here of how many of these algorithmic services they aggregate and represent, all to check and audit that medical claim and assure you upfront as best they can that it won’t be denied or has inaccurate information. For most reading here these are companies you more than likely have never heard of, but again it’s the algorithmic monitoring and transaction fee based  companies that provide this service. Basically if one had an in-house service that did this process, then there would not be a need for additional algorithmic transaction fees or if the decision is made to keep such services in dealing with denials in house.
companies that provide this service. Basically if one had an in-house service that did this process, then there would not be a need for additional algorithmic transaction fees or if the decision is made to keep such services in dealing with denials in house.
There are so many options out there today and the decision making process is complicated and when you look at the fact that the profits go directly to the corporate owner, in this case United, these are profit driven algorithms for sale.
In addition when creating a grouping of services available now we could maybe look at other subsidiaries and what they have to offer, such as HIE services to allow the exchange of medical record information.
Ingenix Acquires Health Information Exchange Services/EHR Provider Axolotl-United Health Group Behemoth Continues to Grow–Subsidiary Watch
Now when making a decision to purchase from one subsidiary open doors for additional purchases from another? It could. As now with grouping all the information in the HIE exchange, are all those involved going to want to purchase the algorithmic services to predict and model medical claims too? So again we are adding on additional transaction fees to accomplish this and they add up quickly for big profits. Now I am going to switch gears and move over into the decision making side to illustrate why you need to hire some good technicians in Health IT who also know their pricing with data base access and transactions as they can save organizations tons and millions of dollars potentially.
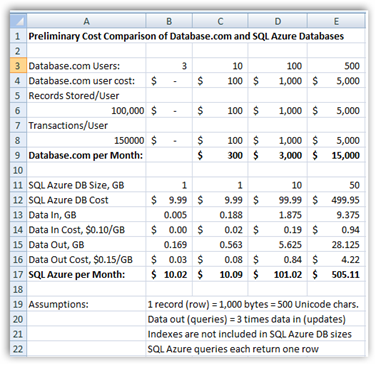
This figures show here in this example come from a “geek” if you will, a programming expert at Oakleaf systems that knows his stuff and did a very simple comparison on how pricing and the cloud can save money. He happens to be working with Azure, which is Microsoft’s cloud based SQL server and did a simple comparison and you can see that a flat charge pricing arrangement versus a transaction fee for each data base accessed has the potential to save "huge'” dollars and also at the same time makes for a real good argument to engage “cloud services” too.
Again this is not related to the discussion above but is merely an access projection on what can be saved and how prudent purchases in Health IT need to be today as there so so many options presented. Does one want to pay for each time records are accessed or is it a better deal to pay a flat fee? You can see the results below and we both agree in this case that dumping the individual transaction fees is the best solution and 15K versus $500 is a big chunk of change, and again this is just a quick sampling to show how transaction fees and their expense add up in a hurry.
Health IT purchases get complicated today so your CIO and CTOs who make these decisions can absolutely be worth their weight in gold. It is all about the value and return on investment today and nobody wants to spend more than they have to but if one is not aware of all the alternatives and perhaps as illustrated above, asking for a flat monthly charge for access versus all those expensive transaction fees, you may be running the expenses right up the flag pole here.
Coming back around to the conversation here today, just remember when contracting for these types of services that they are algorithmic formulas that you need to create an assessment for to determine if they have value for how your business is conducted and don’t over buy as this is what I somewhat refer to as the “Health IT algorithm insurance business” and how much do you need? When you look at who’s showing profits in healthcare today I think you can get the idea and when you see the value that mergers and acquisitions are placing on such companies when purchasing. If you are an employer, you can buy some algorithms to project what cost might be fore employees.
Ingenix (UnitedHealthCare Subsidiary) Creates Desktop Software for Employers to Analyze Employee Benefit Use To Help Cut Costs – More Analytics and Algorithms To Save That Buck
When you get done there, do you want employees to understand their risk assessments, well there’s algorithms for that too so you can tell them if they are a risk to society in costing too much money in short. I find all the services offered to be a huge and sometimes confusing process at times as we can’t even get consumers
Ingenix (Subsidiary of United Health Care) Buys QualityMetric – More Algorithmic Formulas To Choose From To Identify Future Risk and Cost
As a consumer trying to participate in this data dependent world of healthcare today too you might be marketed at the local drug store to enroll in some of the other  additional programs offered too, and look for marketing this year at CES from United.
additional programs offered too, and look for marketing this year at CES from United.
Going to CES This Year–Health Insurance Carrier United HealthGroup Enters Sponsorship Arena
The company has an algorithm for sale in almost any area that may ail you but remember in some of the processes they collect data and sell it for a profit, like your medication records that do not fall under HIPAA, so again there’s a ton of Algos out there in the portfolio for sale and finding value in accomplishing your Health IT goals is a very difficult decision making process today. I tried to focus on the transaction processes here today and didn’t touch on some of the other areas of the behemoth group such as their bank, overseas interests and selling data base information to phama for clinical trials
Again, the transaction fees that run on data systems is not only one of the most expensive aspects of today’s healthcare, but also one that is not seen by most and few other than those who work with such systems are aware of how it exists today. BD
“EHR Physician Advisors work with hospitals to overturn commercial payor clinical denials before a patient leaves the hospital. EHR Physician Advisors have experience in dealing with payors nationwide. This experience and consistency in approach holds payors accountable and reduces the impact of inappropriate denials on accounts receivable. Appealing inappropriate commercial denials at the point of service is a proven method to reduce the impact of denials on a hospital's bottom line.
EHR Physician Advisors will also manage the entire retrospective commercial payor appeal process, including composition of expert, physician-authored appeal letters. EHR Physician Advisors then leverage EHRic's workflow engine to ensure that each case is coded, tracked, and appealed through every payor, state, and regulatory level available.”



0 comments :
Post a Comment