From the website:
Who Should Have a Targeted Prostate Biopsy?:
Because at this time availability is limited for targeted biopsy, we are currently recommending it for men who are suspected of having prostate cancer, but whose tests have been inconclusive, e.g., men with:
- Persistent, unexplained PSA elevation, or
- Prior negative biopsy, or
- Increased prostate cancer gene expression (PCA3 urine test), or
- Apparent low-risk prostate cancer interested in Active Surveillance.
Press Release:
Ground-breaking research by a UCLA team of physicians and engineers demonstrates that prostate cancer can be diagnosed using image-guided targeted biopsy.
Traditionally found only by blind biopsy, a procedure that dates from the 1980s, prostate cancer now appears detectable by direct sampling of tumor spots found using Magnetic Resonance Imaging (MRI) in combination with real-time ultrasound, according to the UCLA study released Dec. 10, 2012 early online for the January 2013 issue of The Journal of Urology®.
The study indicates that the MRI and ultrasound fusion biopsy, which is much more accurate than conventional blind biopsy, may lead to a reduction in the numbers of prostate biopsies performed and allow for early detection of serious prostate cancers.
The study involved 171 men who were using active surveillance to monitor slow growing prostate cancers or men who had persistently elevated prostate specific antigen (PSA) - a protein produced by the prostate that can indicate the presence of cancer – but had prior negative biopsies. The UCLA biopsies were done in about 20 minutes in an outpatient clinic setting under local anesthesia.
Elevations in serum PSA level trigger nearly all of the one million prostate biopsies performed in the United States every year. Annually, about 240,000 new cases of prostate cancer are discovered. Thus, about 75 percent of the biopsies are negative for cancer. However many of those men with negative biopsies but elevated PSA levels may still harbor malignant tumors that were missed by conventional biopsies, said study senior author Dr. Leonard S. Marks, a professor of urology and director of the UCLA Active Surveillance Program.
“Early prostate cancer is difficult to image because of the limited contrast between normal and malignant tissues within the prostate,” Marks said. “Conventional biopsies are basically performed blindly, because we can’t see what we’re aiming for. Now, with this new method that fuses MRI and ultrasound, we have the potential to see the prostate cancer and aim for it in a much more refined and rational manner.”
The new targeting process is the result of four years of work funded by the National Cancer Institute and based in the Clark Urology Center at UCLA.
Since the mid-1980s, prostate cancer has been diagnosed using trans-rectal ultrasound to sample the prostate. Unlike most other cancers, prostate cancer is the only major malignancy diagnosed without actually visualizing the tumor as a biopsy is done, Marks said.
With the advent of sophisticated MRI, imaging the prostate improved and provided a picture of tumors within the organ. However, trying to biopsy the prostate with the patient inside the MRI has proved to be cumbersome, expensive and time consuming. Thus the fusion process evolved, permitting the targeted biopsy to be done in a clinic setting.
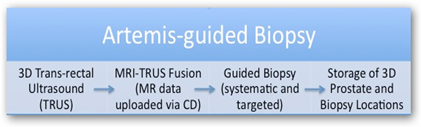
In this study, the volunteers undergo MRI first to visualize the prostate and any lesions. That information is then fed into a device called the Artemis, which fuses the MRI pictures with real-time, three-dimensional ultrasound, allowing the urologist to see the lesion during the biopsy.
“With the Artemis, we have a virtual map of the suspicious areas placed directly onto the ultrasound image during the biopsy,” Marks said. “When you can see a lesion, you’ve got a major advantage of knowing what’s really going on in the prostate. The results have been very dramatic, and the rate of cancer detection in these targeted biopsies is very high. We’re finding a lot of tumors that hadn’t been found before using conventional biopsies.”
Prostate cancer was found in 53 percent of 171 study volunteers. Of those tumors found by the fusion biopsy technique, 38 percent had a Gleason score of greater than seven, which indicates an aggressive tumor, more likely to spread than tumors with lower scores. Once prostate cancer spreads, it’s much more difficult to treat and survival decreases.
Robert Meier, a 58-year-old high school art teacher from Visalia, enrolled in Marks’ study after three prostate biopsies all came back negative for cancer despite climbing PSA levels.
In 2008, Meier tore his rotator cuff and as part of his pre-surgery exam, blood tests were done. His PSA was at six – four or lower is considered normal. His doctor sent him to an urologist, who performed tests to rule out everything else that could be causing high PSA levels, including infection and an enlarged prostate. The doctor found nothing. Meanwhile Meier’s PSA climbed to eight.
A biopsy was performed and was negative. Meier’s PSA jumped to nine and yet another biopsy came back negative. When his PSA reached 11.7, another round of biopsies was ordered.
“These biopsies can be extremely painful and I was put in the hospital several times so they could be done under general anesthesia,” Meier said. “It takes about a month to recover.”
And like his PSA levels, Meier’s anxiety was also rising. If he didn’t have prostate cancer, why were his levels going up?
After a second opinion in Santa Barbara and months of being tested and treated with a medicine designed to shrink his prostate and lower PSA, Meier was referred to UCLA and Marks in 2011. By then his PSA was nearly 18, up more than 10 points in three years. An MRI revealed a prostate lesion and he underwent a biopsy using the Artemis device. He did have cancer, and it was aggressive.
“Dr. Marks told me that I had a cancer that could spread and it needed to come out now,” Meier said. “He told me that at my relatively young age and the severity of the tumor, I had no choice.”
Meier’s prostate and 24 nearby lymph nodes were removed robotically at UCLA in February by Dr. Arnold Chin, assistant professor of urology. Follow up tests show that Meier is cancer free today.
“This program works,” Meier said. “I had jumped through all these hoops and had all these tests with two different doctors and they found nothing. It took UCLA to determine that I had an aggressive cancer that could have killed me. I feel like I was in very good hands at UCLA.”
The UCLA study team included doctor-scientists from urology, radiology, pathology, the Center for Advanced Surgical and Interventional Technology (CASIT) and biomedical engineering.
“Prostate lesions identified on MRI can be accurately targeted with MR-Ultrasound fusion biopsy in a clinic setting using local anesthesia,” the study states. “Biopsy findings correlate with the level of suspicion on MRI. Targeted prostate biopsy has the potential to improve the diagnosis of prostate cancer and may aid in the selection of patients for active surveillance and focal therapy.”
The study was supported by the National Cancer Institute (RO1CA158627). The MRI and ultrasound fusion technology used in the study is described in a video posted here.



0 comments :
Post a Comment