As the President said this week, it’s all about doing the math and when it comes to insurer rate increases, well that’s math and business intelligence algorithmic formulas are used by the carriers to go forward with their requests for rate hikes and by law anything over 10% needs to be approved. Last year HHS told WellPoint to bring their algorithms for rate increases to Washington over the proposed increases in California.
HHS to California Blue Cross – Bring Your Algorithms to Washington And Explain
Some carriers such as Blue Cross also uses behavioral analytics to work with wellness programs and where and who has access with some of those we don’t know at times and some like Red Brick are smack a bit of big brother with some of  their devices and discounts given to employees who participate to save money.
their devices and discounts given to employees who participate to save money.
WellPoint enters wellness program partnership With Red Brick – Behavior Based Health Insurance
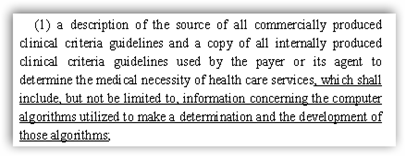
In some states though, some governments are “getting smart” and realize this is the “Algo Game” and are asking carriers for their formulas.
New Jersey Legislature Getting Smart– Bill to Modify Claim Procedures to Include Asking For Insurance Company Algorithms-Bill A3334
I think we are going to see a lot of explaining here as transparency moves through and hopefully some of the grant money will help that along with deciphering the Algorithms used for calculations as they have been wrong. We can hardly forget the AIG algorithms that were in fact pretty dirty and there will be more. These algos helped create credit ratings…..and this goes back to 1987 and the process has been building since with too many trusting individuals on the consumer side being fleeced. BD
AIG: You Bring the Nerds and the Algorithms and I’ll give you a AAA Rating…a little history from 1987
WASHINGTON – The Department of Health and Human Services (HHS) granted $109 million Tuesday for states and the District of Columbia to fund reviews of health insurance rate hikes.
“We’re committed to fighting unreasonable premium increases and we know rate review works,” said Kathleen Sebelius, HHS secretary, in a statement. “States continue to have the primary responsibility for reviewing insurance rates and these grants give them more resources to hold insurance companies accountable.”
As of September 1, 2011, the Affordable Care Act requires health insurers seeking to increase their rates by 10 percent or more in the individual and small group market to submit their request to experts to determine whether the rates are unreasonable. The ACA also requires insurance companies to publicly justify unreasonable premium rate increases. The goal of these provisions is to bring greater transparency and accountability to the process.
HHS also released a new report Tuesday entitled "Rate Review Works," detailing how previous rate review grants are fighting premium hikes and helping make the health insurance marketplace more transparent.
Improve transparency and consumer interfaces: Twenty-eight states and the District of Columbia are proposing to use grant funds to improve consumer interfaces, such as developing a rate review home page at the Department of Insurance website and providing opportunities for consumers to comment on proposed rate hikes via the website.
http://healthcarefinancenews.com/news/hhs-grants-109m-help-keep-insurance-premium-hikes-reasonable



0 comments :
Post a Comment