Update: The penalty for non participation has been removed. Follow the money as I always do and when you see the University needing money and their wellness partner WebMD needing money, strict enforcement tactics were tried as they wanted to get all the data they could in order to be able sell it. This is an epidemic in the US and we need to excise tax and license all data sellers. The data selling epidemic is also creating a lot of additional flawed data in system everywhere.
Implementation is everything whether it is Wellness or some other type of plan and it was just last year that the WebMD CEO resigned and ended it’s search for a buyer due to loss of advertising revenues. 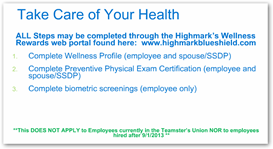 I understand as stated here that WebMD Health Services operates separately but all divisions have a responsibility to put profits down to the bottom line of any corporate structure. In 2011 there was the class action suit filed against WebMD for potential inside trading and recently another company MyMedicalRecords.com filed a patent infringement against the company.
I understand as stated here that WebMD Health Services operates separately but all divisions have a responsibility to put profits down to the bottom line of any corporate structure. In 2011 there was the class action suit filed against WebMD for potential inside trading and recently another company MyMedicalRecords.com filed a patent infringement against the company.
WebMD CEO Resigns and Company Ends Its Search for a Buyer–Advertising from Pharma At Lower Levels
If one is a consumer and reads the news headlines as such might cause a member to ask some questions about the new program, I would but I look at subsidiaries of a lot of healthcare companies and try and see what they do and attempt to figure out their role in the big corporate group, who wouldn’t right? I think shareholders might do some of this when it comes to investing.
Anyway you add all of this up with somewhat of a “strong arm” approach to wellness and one might say “what’s going on here”. Here’s what I could find on WellPoint on their SEC listings here for 2009 and 2004. I couldn’t find anything more recent but that doesn’t mean I didn’t miss something. Part of the issue could be at the SEC though as it was reported this week that pencils and hand calculators were being used at the SEC to file company information instead of the automated XBRL automated digital system that allows for tagging and indexing what companies file with them.
In February of 2012 we had the big announcement to where Highmark was one of the Blue Cross companies that purchased NaviNet to give doctors access to insurance claim information, a medical records program and more. If you read the information below with all the technology company subsidiaries, the lines get gray for the average consumer to figure what’s going on half the time. As you can see now we have some medical record systems in the mix too, and so an insurance company has an interest in meaningful use as they own the company when it comes to doctor’s incentives. Aetna was and probably still is a big user of NaviNet so they are also a client in here too.
to give doctors access to insurance claim information, a medical records program and more. If you read the information below with all the technology company subsidiaries, the lines get gray for the average consumer to figure what’s going on half the time. As you can see now we have some medical record systems in the mix too, and so an insurance company has an interest in meaningful use as they own the company when it comes to doctor’s incentives. Aetna was and probably still is a big user of NaviNet so they are also a client in here too.
Blue Cross/Blue Shield Insurers and Highmark Acquire NaviNet Transactional Portal And Medical Records Vendor–Subsidiary Watch
I look at it this way in the fact of I follow data trails and perhaps some of the information gathered here will end up giving WebMD some additional data or data profiles to sell too. A lot of wellness companies generate data for sale in on form or another, de-identified or otherwise. You really have to give some thought as we also have Blue Cross and other insurers buying your MasterCard and Visa records from the banks to monitor and see if you are beginning to buy clothes a size larger (those are the words of Blue Cross not me and I think they could be doing more queries with the data) …more data for sale and more profits there…cha ching..not to mention the scandal with the former CEO that hit Highmark with his love triangle. We have the “junk food” data story too that was in the news recently.
Ok so with some of this going on is it any wonder the participants with the approach being used questioned what’ going on..I don’t think so as the US has a huge data selling epidemic going on and that’s the first thing I would think of is who might be getting some data for sale and profit. Insurers are big in this game and we know WebMD needs some money, so again why this kind of “strong arm” approach? We also had this relative to competition between the hospital and the insurers.
wonder the participants with the approach being used questioned what’ going on..I don’t think so as the US has a huge data selling epidemic going on and that’s the first thing I would think of is who might be getting some data for sale and profit. Insurers are big in this game and we know WebMD needs some money, so again why this kind of “strong arm” approach? We also had this relative to competition between the hospital and the insurers.
Hospitals and Insurance Company Competing for Patients In Pittsburgh–Contracts In Question
Back in 2009 WellPoint partnered with Red Brick which is another wellness program that is a client of Optum (UnitedHeathcare) and uses their analytics. The Red Brick Wellness CEO came right out of UnitedHealthcare. Seeing some patterns here? It comes back to data, data and more data and Red Brick for one was one of the first to bring device out to collect data with their Target contract a while back and if you want to really look into the business models of consumer apps and devices, read this post about Intel and how deep some of these financial models go with business models and money.
WellPoint enters wellness program partnership With Red Brick – Behavior Based Health Insurance
In view of what I just grouped together from prior posts I have done and with this strong arm approach, no doubt questions arise and folks want to know “why”…data, data and more data I think is a big part of it here and this adds to what we all fear, inequality modeled with segmentation. Again when all the wellness rage began I had my suspicions way back in 2009 but again I look and try to figure out what they are doing to do with all that data and what subsidiaries might communicate with other subsidiaries with data , being I used to develop and worked a lot with data bases and the process of doing that involves looking for value. BD
Penn State administrators quietly introduced the plan, called “Take Care of Your Health,” this summer in the deadest part of the academic calendar. But that didn’t prevent some conscientious objectors from organizing a protest online and on their campuses, culminating last week in an emotionally charged faculty senate meeting. The plan, they argued, is coercive, punitive and invades university employees’ privacy.
The plan requires nonunion employees, like professors and clerical staff members, to visit their doctors for a checkup, undergo several biometric tests and submit to an extensive online health risk questionnaire that asks, among other questions, whether they have recently had problems with a co-worker, a supervisor or a divorce. If they don’t fill out the form, $100 a month will be deducted from their pay for noncompliance. Employees who do participate will receive detailed feedback on how to address their health issues.
What’s more, they argued, the online questionnaire required them to give intimate information about their medical history, finances, marital status and job-related stress to an outside company, WebMD Health Services, a health management firm that operates separately from the popular consumer site, WebMD.com.
Many employers — 36 percent of large companies with wellness programs — use financial incentives to nudge employees to participate, according to a new study by the Kaiser Family Foundation. But Penn State’s plan differs from many in that uses a stick, not a carrot, to sway employee behavior.
James M. Ruiz, an associate professor of criminal justice and a retired police officer, told me that he objected because he felt Penn State had failed to do basic due diligence, signing off on the wellness plan without using the rigorous scientific methods that faculty members routinely require of students. He has urged the faculty senate council, of which he is a member, to ask the university to delay the program for one year so that administrators may consult outside experts on wellness plan efficacy, data security and privacy.
http://www.nytimes.com/2013/09/15/business/on-campus-a-faculty-uprising-over-personal-data.html



0 comments :
Post a Comment