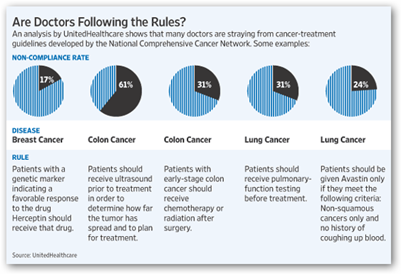
Back in February of this year United Healthcare sent a report out to Oncologists across the country with a small study relative to following procedures and rules and added some cost analysis. After reading this article in the New York Times there seem to be some open lines of communication and payment structures seem to be flexible. 
United HealthCare Sends Oncology Reports to Doctors – Assessing Cancer Treatment Rules Compiled by Ingenix
Aetna has a group of MDs in Texas they are working with and Blue Shield is working with Hill Physicians in northern California with a group of state workers. Some of those oncologists are being rewarded for saving money but Hill is making sure the doctors get paid even if the treatments become expensive. A Harvard professor is a little concerned over the reward system as he feels it could lead to errors.
One oncologist referred to an example to where a less expensive treatment required more time versus a more expensive treatment that required less time so there’s another question on the table that needs to be entertained as well as far as the amount of time spent by the patient getting care. The main goal here though too is to not restrict care due to cost of course and hopefully something will be worked out so the out and out cost of care doesn’t rule the type and quality of care deemed necessary by the doctor. BD
Several large health insurers, including UnitedHealthcare and Aetna, are focusing on one of the country’s most costly diseases: cancer.
The insurers have begun tightening oversight of the care provided to patients with many different types of cancer, hoping to lower expenses by experimenting with new ways to pay specialists.
UnitedHealthcare plans to announce on Wednesday a one-year project with five oncology practices, offering doctors an additional fee. The new fee is meant to encourage doctors to follow standard treatments rather than opting too often for individualized and unproven courses of therapy, which can include the most expensive drug combinations. By proposing a different type of payment structure, companies hope to lower doctors’ dependence on a system that generates substantial sums for cancer specialists who routinely favor top-of-the line treatments.
Regional insurers in some states, including California, Washington and Pennsylvania, are negotiating similar limits with doctors and their clinics. WellPoint, another large insurer, is developing a way of paying oncologists to coordinate and manage patient care.
Still, detractors worry that these changes could represent a first step toward denying patients additional treatments or the latest chemotherapy regimen based solely on the cost. In other words, they argue that even if oncologists still decide what course of treatment a patient should receive, as these new plans allow, the new effort could be viewed as a move toward rationing care at the end of life.
For example, doctors could choose less expensive therapies. When an oncologist considers different treatments, “it’s hard not to look at price differentials,” Dr. Bach said. In treating one type of lung cancer, for example, doctors can select from as many as eight treatments that are generally considered appropriate. Their costs under the Medicare program range from about $1,300 to $7,000 a month.
Health Insurers Test New Payment Incentives for Cancer Care - NYTimes.com



0 comments :
Post a Comment