In short, this is a mess! There were 5 levels of consultations formerly and now they have been crashed in to 3 levels, so in plain English 2 are gone. What does this  mean in particular for specialists billing, lower payment and hospitals too. With this article we now have conflicting advice from Medicare contractors, so what’s a doctor and a hospital to do, send claim and cross fingers? Back in December I posted about the changes and now that there is time for actual billing to occur we seem to be seeing a lack of collaboration along these lines. 99241-99245 (outpatient/office) and 99251-99255 (inpatient) are gone for 2010 for Medicare claims.
mean in particular for specialists billing, lower payment and hospitals too. With this article we now have conflicting advice from Medicare contractors, so what’s a doctor and a hospital to do, send claim and cross fingers? Back in December I posted about the changes and now that there is time for actual billing to occur we seem to be seeing a lack of collaboration along these lines. 99241-99245 (outpatient/office) and 99251-99255 (inpatient) are gone for 2010 for Medicare claims.
Medicare Eliminates Consultation Codes in 2010 – Adds Modifier to Distinguish Providers
What also adds to the confusion here is that some commercial insurers still allow for the full bank of 5 consultation levels, so if a claim is submitted with Medicare as a secondary with one of these codes, well you guessed it, the secondary portion could get denied. If you are a patient, expect some delays perhaps on getting your claims paid, this is not the doctor’s fault on this end of the spectrum.
A related article offered these suggestions:
1. Consultation codes 99241-99245 (outpatient/office) and 99251-99255 (inpatient) have been eliminated. Tele-health consultation G-codes (G0425-G0427) will not be eliminated.
2. Use codes for new (99201-99205) or established (99211-99215) patients to replace consultations in the office/outpatient setting.
3. Codes in the inpatient hospital setting (99221-99223) should be used to replace inpatient consultation codes (99251-99255), and for nursing facility consultations use codes (99304-99306).
4. To distinguish the difference between the admitting physician of record from the consultants for initial hospital inpatient and nursing facility admissions, Medicare will develop a modifier. Check with your local carrier for more information.
5. Payments for all Evaluation and Management codes have been increased in an attempt to offset the fees lost from the elimination of consultation codes.
Now we wait until CMS can offer guidance so the miracle of getting paid for services rendered appears. It appears the lower level consults look ok in Medicare’s book. The AMA guidelines state to always bill the initial service prior to a subsequent visit, which makes sense to bill in the series of events that take place; however who says logic is always the way to go? One contractor states that when reporting a subsequent visit, even though this perhaps is not what a provider may want or should do, it formats the data submitted in a way that Medicare can process and pay the claim more efficiently, go figure! It further states that this Medicare contractor will not find fault with submitting using this procedure. Are you confused yet?
If billing a 99499, providers should put a note on the claim to indicate documentation can be provided by request! So how do we get this over to code 99231? For  those not hip to all of this jargon, 99231 means a lower decision making process compensation. In plain English, did your doctor spend 5 minutes with you and ask you to stick your tongue out and say “aaaa” or did the doctor sit down and discuss a full explanation for a potential surgical procedure you may need like lumbar implanted devices, how they work, the type of surgery, anticipated results, recovery time, the type of device, how it will help cure or treat your condition, and basically advise you as a patient as to their recommendations and then, let’s add on some alternative solutions too, maybe a treatment with drugs instead! This is big exaggerated to a degree with my examples but wanted to define how consultations are all over the spectrum.
those not hip to all of this jargon, 99231 means a lower decision making process compensation. In plain English, did your doctor spend 5 minutes with you and ask you to stick your tongue out and say “aaaa” or did the doctor sit down and discuss a full explanation for a potential surgical procedure you may need like lumbar implanted devices, how they work, the type of surgery, anticipated results, recovery time, the type of device, how it will help cure or treat your condition, and basically advise you as a patient as to their recommendations and then, let’s add on some alternative solutions too, maybe a treatment with drugs instead! This is big exaggerated to a degree with my examples but wanted to define how consultations are all over the spectrum.
On this portion, even as a patient you can relate to the difference here with the amount of time spent, research and levels of recommendations by your doctor, and the codes are how they get paid. The very high levels of decision making and time spent are gone and now we have 3 levels to bill, and with consultations there’s back up information required too so the doctor substantiates his time to bill for this. There are names for this type of documentation, like a “review of systems”, and an “H and P” as they are known with documentation in a chart, so sometimes when claims are submitted there is a request for the doctor after the claim has been sent off, so send additional information too, longer processing time for the claim to be processed and payment delays.
“One other simple way to look at this for a layman’s comparison is like being a student and having the option to be graded an A, B, C, D, F on a test. A new system only allows for B, D or F, so the A and C categories are gone. I included this tidbit here to help those outside of this, like patients, to perhaps understand a tiny portion of how your “codes” work with healthcare and how the doctor’s are compensated. To elaborate a little more on this simple example, we still have some teachers that use all 5 and all this has to mesh together so where do the A’s and the C’s go now and the Principles of the schools get confused too, as to how can we overall evaluate students with the same standards? Again, I hope this little example helps explain a little on tiering levels of decision making and treatment processes here and what it means to your doctor.”
We’re not done yet! Ok now comes the time for the companies that sell anti-fraud software to run algorithms and detect fraud on claims? Oh boy, what is the next potential area of yet further delaying a claim? Now from what you have just read can you see formulas and algorithms applied to these types of medical claim. Even if they are not flat out denied, they will be pulled over for additional analysis with running additional formulas and algorithms, in other words why were the bills coded this way? These are companies like Ingenix that will further study every inch and nook and cranny of the claim submitted and sometimes this can be done after the fact too, when the claim has perhaps already been paid.
We have all heard those stories on the news about how an insurance carrier comes back after the fact and denies payment due to what was considered either “fraudulent” activity or some perhaps “false positives” from the algorithmic formulas. These are some of the stories that were documented in Sicko for one example. You can bet there are programmers working to derive some new algorithms in this department, maybe almost as I am writing here. Your doctor and hospital are just trying to get paid, but again with conflicting rules and opinions here between Medicare and insurance companies, who’s algorithms do you apply, and when and where? Everybody is not on the same channel here, so again there can be some false positives generated in the processes and just flat out mistakes and miscalculations too. If a carrier still accepts the 5 levels and Medicare only has 3 levels and they get billed on the same claim with Medicare as a secondary, well Houston we have a problem.
This is just an example of the complicated rhetoric that goes on with providers trying to “code” and get paid for their time so if you are not aware a a patient, I hope perhaps this may have provided some useful information, and in the meantime for all the providers, they are sitting on the edge of their seats to see how new decisions, laws, regulations are going to simplify this process so they can “spend more time with seeing patients and providing better care”, what a novel idea if in fact this payment process could be simplified once and for all. If nothing else here, this certainly makes one big case for the further development of standards in medical billing, that’s for sure. BD
Medicare’s transformation of consultation coding has taken a new twist in the arena of lower-level hospital consults.
Without national guidance from CMS, different Medicare contractors are giving conflicting instructions to providers on billing for consultations that don’t qualify for any of the three evaluation and management (E/M) codes now used for inpatient consults. None of the instructions suit compliance officials, who cite the financial and compliance drawbacks.
A CMS spokeswoman tells RMC that the agency “will be providing additional guidance soon.” Until then, Medicare contractors have been told to do as they see fit.
The challenge with billing lower-level consultations emerged as CMS eliminated consultation codes, including inpatient consult codes (CPT 99251 to
99255). Effective Jan. 1, 2010, physician consults are billed to Medicare under regular E/M codes. For example, consulting physicians will use 99221 to 99223 for initial inpatient evaluations and 99231 to 99233 for subsequent hospital visits. That means five levels of consultation services must now fit into three levels of services.
As it turns out, some physician consults wind up in a black hole. They don’t rise to the level of a 99221 initial inpatient visit because the patient exam, history and/or medical decision making is not complex or comprehensive enough (according to Medicare E/M documentation guidelines). But with CMS apparently planning to keep writing checks for low-level consults, Medicare contractors had to devise ways to process these claims.
“Doing a manual review goes against everything” that HHS has been emphasizing — “budget reduction, more electronic and less paper,” says Kristin Scarcella, assistant director for reimbursement, compliance and education at the University of Michigan Professional Billing Office.
It’s unrealistic to expect physicians to make different coding selections for Medicare versus private payers, which still use CPT consultation codes, without a crosswalk, she says.
Medicare Contractors Use Conflicting Rules on Consultations; CMS to Issue Guidance Soon


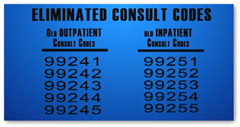 99255). Effective Jan. 1, 2010, physician consults are billed to Medicare under regular E/M codes. For example, consulting physicians will use 99221 to 99223 for initial inpatient evaluations and 99231 to 99233 for subsequent hospital visits. That means five levels of consultation services must now fit into three levels of services.
99255). Effective Jan. 1, 2010, physician consults are billed to Medicare under regular E/M codes. For example, consulting physicians will use 99221 to 99223 for initial inpatient evaluations and 99231 to 99233 for subsequent hospital visits. That means five levels of consultation services must now fit into three levels of services.
You know this whole method of coding and billing for Medicare reminds me of being in a wood boat that is constantly springing leaks and the only thing to stuff in the holes to stop the leaks are newspapers. The water stops coming in and then the newspaper gets soggy and the water just seeps through. Eventually the paper is so saturated it just blows out and the hole opens again. I'm afraid unless they figure out a better way to code and bill. We will all go down with the Medicare financial ship.
ReplyDeleteTony
http://www.bontemedical.com/blog